Share
Editor’s Note: Parts I, II, IV, and V of this series can be found online on the Counselor blog. Part III was published in the April 2021 issue of Counselor magazine in the same column.
In part five of this series, we covered the little-known trigger recovery process. In this final article, we will explore relapse warning signs and provide a simple, three-part, relapse prevention education series that is easily administered by any addiction professional. Remember that despite the danger, many addiction professionals focus merely on teaching the tools of recovery to individuals once craving hits, rather than preparing them beforehand on how to avoid falling into the craving cycle in the first place. In this series, we are doing just that: demonstrating how to help our patients minimize the frequency of entering the craving cycle. We are accomplishing this by focusing on setup behaviors and trigger events, the two primary criteria that contribute to the craving cycle. By utilizing this information, patients can significantly reduce craving frequency.
Warning Signs
In his book with Merlene Miller titled Staying Sober: A Guide for Relapse Prevention (1986), Terence Gorski coined the term “relapse warning signs.” He writes that he conducted clinical interviews with 118 recovering alcoholics and drug addicts who had completed a twenty-one- or twenty-eight-day program, recognized they were addicted, intended on staying sober postdischarge with the help of AA and outpatient counseling, and eventually relapsed. By compiling the responses of these subjects identifying the warning signs that might have told them they were on the road to relapse, Gorski came up with a list of the most common responses—hence, the creation of Gorski’s famous thirty-seven warning signs of relapse (Gorski & Miller, 1986, p. 140).
The importance of warning-sign identification is based on the idea that relapse is not the action of picking up drugs or alcohol, but rather is a process that happens over days, weeks, months, or even years and finally culminates in the actual use. This is good news for people in recovery, because the intention is to avoid the “picking up” part. There are many warning signs that can tell individuals they are in the relapse process, and if they can identify the signs when they occur, they can intervene before substances are actually obtained.
It is important that our patients identify their warning signs early in recovery, because when they are in the relapse process there is a tendency to have distorted thinking, which makes identification of these signs extremely difficult. If individuals regularly view a list of warning signs they compiled when they were not inside the relapse process, they will be able to identify symptoms they might not otherwise be capable of recognizing.
Warning signs and triggers are not the same, although there can be much overlap between them. Remember, a trigger is something that is connected to individuals’ using and is what activates the craving cycle. A warning sign, on the other hand, is something that indicates that people may be on the road to relapse. For example, seeing using friends can be both a trigger and a warning sign. As a trigger, seeing using friends often occurs simultaneous to or just before using drugs or alcohol—a connection is made between seeing using friends and drinking or using. This connection is what activates the craving cycle and makes it a trigger. As a warning sign, seeing using friends may also indicate oncoming relapse because patients who expose themselves to such people are putting their sobriety in danger. Being exposed to such dangerous situations is clearly a warning sign that these patients are setting themselves up for relapse.
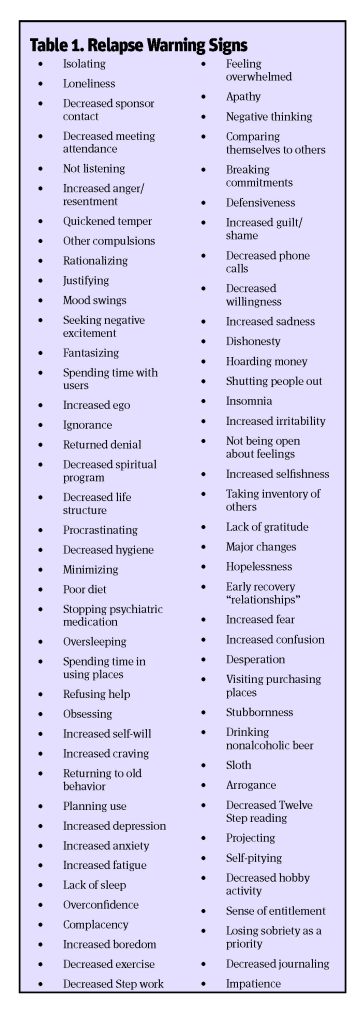
In my relapse prevention education series, patients are educated on warning signs. Additionally, using the same brainstorming method described in the triggers article (i.e., article five in this series, found on the Counselor blog), patients are asked to identify warning signs they experienced that might have indicated they were on the road to relapse. If they have no relapse history, they are asked to identify what warning signs they think might occur for them prior to relapse. As with the exercise described in the triggers article, the warning signs patients come up with are first written on the board, then written down on paper, copied, and distributed. I would have them highlight about six to eight warning signs that might particularly apply to them and to review the list on a daily basis. Table 1 is a list of warning signs I compiled in a similar fashion to my compilation of triggers. If you have read Gorski’s and Miller’s Staying Sober (1986), you will notice much overlap in these and his original thirty-seven warning signs of relapse.
I really tend toward the brainstorming exercises as previously described because they get our patients thinking. We want them thinking for themselves and the problem-solving skills that result from it. As we conclude this series, I want to recommend a simple, three-part, relapse prevention education system that includes this exercise.
The Tools of Recovery
No relapse prevention system is complete without educating patients on the tools of recovery and how to apply them to prevent relapse. They need to know what to do when they have a craving or have uncomfortable feelings they previously escaped by using alcohol and drugs. Therefore, along with the triggers and warning signs education and lists, clinicians can perform a brainstorming exercise about the tools of recovery as well. We might ask a group, “Based on what you have learned thus far in treatment, and perhaps from previous treatment episodes, what are the tools that are common used by people who succeed at long-term recovery?”
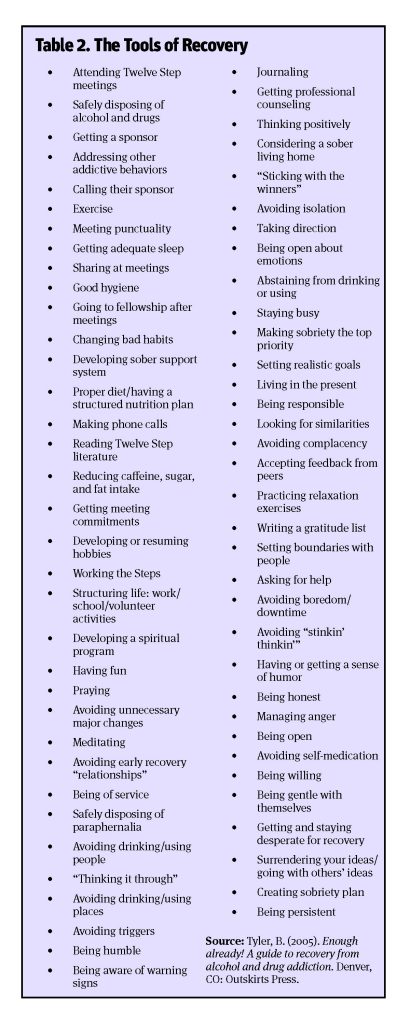
As we are doing any of these brainstorming exercises, it may go silent after a while, but that is okay. Why? Well, when it is quiet they are thinking, and that is what we want! If they are struggling coming up with some of the main tools of recovery, we can point them toward the ones we want to make sure are on the list. Once the list is complete, we can take some time to clarify how certain tools are utilized and to answer any questions they may have about them. Again, this is a brainstorming exercise during which clinicians will write down what patients come up with on the board, have them written down on paper by one of the patients, make photocopies of the list, and distribute the copies to the group. Table 2 on the following page is a list of ingredients for recovery compiled in a similar fashion to my compilation of warning signs in Table 1.
In weeks two and three of the education series, we can then conduct the triggers and warning signs brainstorming exercises as previously described. Once complete, patients will have a copy of the tools of recovery list, the triggers list, and warning signs list. We should encourage our patients to keep these lists accessible so they can be viewed on a daily basis. We might also recommend putting the three lists next to their morning meditation book and to make it part of their morning recovery ritual: starting their day with the morning meditation reading and then reviewing these three lists. This review will not take more than five minutes per day and is an invaluable resource to patients’ recovery. I cannot overemphasize the value of the following for our patients:
- Reviewing a list of recovery tools that are used for successful, long-term abstinence allows for:
- Daily education on what to do to stay sober
- A daily reminder of the tools they have not yet implemented, but plan to
- A daily reminder of tools they may have been using previously, but stopped
- Reviewing a master list of triggers (with highlighted items that particularly apply to them) allows for:
- A daily review of triggers to keep this phenomenon on the forefront of their mind
- Reviewing their day to see if they will be exposed to any such triggers so they can arrange to avoid them or create a sobriety plan if they cannot
- Reviewing a master list of warning signs (with highlighted items that particularly apply to them) allows for:
- The identification of any warning signs that indicate they are on the road to relapse
- Keeping personalized warning signs on the forefront of their mind so they can prevent slippage into them
- Exposing the source of craving if they are in the craving cycle so they can intervene effectively
Summary and Conclusion
The craving cycle—obsession, compulsion, physical craving, and drug-seeking behavior—happens to all alcoholics and addicts and always precedes relapse. So, along with providing tools of recovery they can use when the craving cycle hits, we need to help them avoid getting to the craving cycle to begin with. How we do that is by educating them on physical, psychological, and social setup behaviors as well as thinking, feeling, acting, and relational trigger events. This way they will be able to avoid getting into the craving cycle as often, and thus decrease their chance of relapse. Some of this information can be formalized in a brief relapse prevention education series utilizing a brainstorming technique resulting in lists containing the tools for recovery, trigger events, and warning signs, which our patients can review on a daily basis—an excellent adjunct to anyone’s daily program of recovery.
I hope this course will add to your repertoire of relapse prevention tools, and that you continue honing your skill base in treating this dreadful disease. Thank you for all you do for our patients and I hope to see you at a conference someday!
References
Gorski, T. T., & Miller, M. (1986). Staying sober: A guide for relapse prevention. Independence, MO: Herald House/Independence Press.
About Me
Bob Tyler, BA, LAADC, CADC-II, has been working in inpatient, residential, and intensive outpatient levels of care since 1990. He serves as compliance officer at LA CADA, is owner of Bob Tyler Recovery Services (consulting, CD private practice, training), is past president of CAADAC, and is on faculty at LMU Extension in the AOD Studies Program. He authored the EVVY Award-winning book, Enough Already! A Guide to Recovery from Alcohol and Drug Addiction, and has produced several educational DVDs shown in over one thousand treatment centers across the country, including Craving and Relapse.












 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.