Share
Accessible technology has credibly established its place in health care, improving service delivery, streamlining processes, and extending the availability of support when funding and staffing levels present a challenge to delivering an effective service. A successful example of this is the British National Health Service (NHS) application that allows patients to order prescriptions, message their doctors, and validate their COVID-19 vaccination status (NHS, 2021), all from a mobile device, without the need to engage with service professionals.
Chatbots are a leading type of accessible technology available on any Internet-enabled device. Their use in health care is an area of significant and growing interest (Ogilvie et al., 2021), which is understandable given their ability to simulate a real-time, “human-like” conversation in any given area of care if they are accurately programmed to do so. Chatbots offer a type of human-computer interaction that makes a systemized conversation seem authentic, engaging, and comparable to a human-to-human interaction. They connect users to the content being delivered using natural linguistics, which are both familiar and comfortable for the end users to interact with (Adamopoulou & Moussiades, 2020). In mental health care this capability has been recognized for the therapeutic benefit that a humanized system agent can afford people who need to interact in a way that they feel provides an understanding relationship (Vaidyam et al., 2019).
Chatbots form a distinct branch of artificial intelligence (AI) and are an area undergoing rapid technological advancement. Chatbots are deployed across a multitude of sectors to take on roles traditionally undertaken by human agents (Adamopoulou & Moussiades, 2020). The health care sector is no exception, and as AI capability improves and chatbots become more ingrained in our daily lives, a new revolution is perhaps being observed—perhaps one where systemized agents can influence the future delivery of health care services. What can be said with certainty is this: the developmental stage of the life cycle new chatbots exist in is undergoing meaningful refinement in the functions and services they perform.
An Age Group Primed for a Technological Solution
In drug and alcohol addiction recovery, relapse is commonly understood to be the point when individuals break a sustained period of abstinence. Those working within the addiction field sometimes break this down further to differentiate between lapse and relapse—“lapse” describing an acute interruption to abstinence, often signifying an impending relapse, and “relapse” itself indicating a return to more chronic and entrenched substance-using behaviors (Baumeister & Nadal, 2017). In this respect, relapse is often considered a process where thinking patterns and subsequent behaviors offer warning signs of failing recovery. If these signs are left unchecked, there is a significant increase in the risk of addicts moving from recovery back to their previous level of addiction (Melemis, 2015).
Statistics show that in England the most common age to engage with addiction treatment services is between thirty to forty-four (Public Health England, 2020). As a demographic, this age group is also strongly linked with addiction-related deaths. In the United States, data gathered in 2015 showed that 72.7 percent of cirrhosis deaths for this age group were alcohol related (NIAAA, 2022). Similar findings have been reported for drug-related deaths. For example, in northern Europe a continuing year-on-year upward trend has been seen in drug-induced deaths, with this age group the most affected (EMCDDA, 2021). From this it can be reasoned that, as a group, thirty- to forty-four-year-olds are most affected by the adverse effects of addiction, and subsequently most likely to engage with support services in a bid to extract themselves from its damaging consequences.
By engaging with addiction services, addicts are selecting a course of action that, if upheld, will see them transition to recovery, providing they can weather the challenges that may pose a risk to continued abstinence. Individuals within this cohort are typically technologically adept. They are a generation that has matured alongside a technological revolution, which has seen basic mobile phones evolve to multifaceted smartphone devices that stream content at great speeds and can perform functions that were once the remit of science fiction. This age group have been instrumental in social media becoming a primary platform for shared discourse, also playing their part in the collective movement driving forward the applied use of AI (Elena-Bucea et al., 2021).
Why Chatbots for Addiction Recovery?
The use of chatbots in the field of addiction is an emerging area of interest. To date, contribution to the overall body of work on the subject is limited when compared to other areas of health care (Adamopoulou & Moussiades, 2020; Abd-alrazaq et al., 2019). This was evident in a recent review that showed chatbots in this field to be both underrepresented and underdeveloped (Ogilvie, Prescott, & Carson, 2021). This proffers an opportunity to realize the untapped potential in applying this branch of AI to support people with a history of problematic drinking and drug use. Also, it raises the question of how chatbots could and should be used to offer this support.
Try Foxbot!
Foxbot forms part of larger project to disseminate positive addiction recovery therapy (PART) via online channels to expand availability beyond a group setting. To try Foxbot, visit the website www.positivelysober.org, where you can also see some of the work currently underway on PART.
Challenges to recovery can happen at any time, often arising in unanticipated ways such as a reaction to an event, external stimuli, or an emotional response (Melemis, 2015). Chatbots are available 24/7, providing individuals have access to an Internet-enabled device. Having a service that is instantly available and exclusive to people in addiction recovery is of considerable worth to those who need addiction-informed support at unpredictable times, like when individuals have been triggered by something stressful that they once would have used drinking or drugs as a coping mechanism for (Turner et al., 2018).
Some may ask how chatbots differ from helplines or online mutual-support meetings that are available 24/7 as well. Firstly, people with a history of addiction often feel stigmatized, judged, embarrassed, and/or ashamed, which can present barriers to speaking about their problems (Matthews et al., 2017). Systemized agents remove this barrier as they are judgment free, their only agenda being that with which they are programmed. Secondly, chatbots are convenient and can be accessed at the point of need with no explanation as to why help is being sought. This reduces pressure on the individuals seeking support, as they do not have to replay the event or situation that presented the challenge for which they are seeking help.
Chatbot development platforms are now relatively simple to access and use, meaning chatbots can be implemented with minimal cost and effort, yet still benefit from sophisticated AI technology. Additionally, their programming can be informed by field experts and the knowledge base created so that it is conversant with material provided from prospective users, essentially seeing the production of a recovery resource designed for addicts by addicts. This removes the reliance on technical experts and system designers who tend to focus on the quality of the system, as opposed to the importance of its content (Janssen et al., 2021).
A Solution Designed to Mitigate the Risk of Relapse
The idea of using technology to amplify well-being and maximise potential is a relatively new area of study and a novel direction to consider computing solutions in addiction recovery (Calvo & Peters, 2017). In health care, systems that require patient interaction often focus on improving or extending service provision; they are designed for treating and diagnosing conditions as well as educating users on health-related matters. This does not leverage technology for the greater social good of maximising human potential and well-being (van Gemert-Pijnen et al., 2018; Calvo & Peters, 2017). To date there is little evidence to say that the proliferation of digital technology has acted as a proxy for improved well-being (Calvo & Peters, 2017). It is therefore reasonable that interest has waned in the unfulfilled potential of solutions explicitly designed for this purpose.
Taking the concept of positive computing, applying theoretical input from positive psychology, and utilizing knowledge from potential users and field experts, the design of a new chatbot called “Foxbot” was formulated. Foxbot is targeted at people in addiction recovery with the objective of providing positive recovery interventions (PRIs) that reduce the immediate risk of relapse and provide users with ideas that will bolster their recovery and help remove them from the immediate risk of relapse (see Figure 1). The design of Foxbot was split into two categories: the characteristics of the chatbot and the PRIs delivered by the chatbot.
Foxbot: A Chatbot with Character
Positive relationships and social connection are important components of well-maintained recovery—they affect how people experience and interact with their surroundings, not only supporting recovery, but also making it enjoyable (DiClemente, 2018). Foxbot was designed with this in mind, being given a friendly manner and character strengths that complement the role of a recovery friend.
In positive psychology, character strengths define the positive parts of people’s personalities. In total there are twenty-four character strengths individuals may exhibit to a greater or lesser extent. Of these, the top five strengths, known as “signature strengths,” describe the most positive aspects of character (Niemiec, 2018; VIA Institute on Character, n.d.). They pinpoint what someone does well and represent the aspects of personality that make them engaged and authentic (Niemiec, 2018). To anthropomorphize Foxbot and authentically construct the identity of a recovery friend, it was decided to assign signature strengths in the design of the systemized agent. The selected strengths were gratitude, self-regulation, social intelligence, humor, and creativity.
- Gratitude to solidify the idea that recovery and connection is something to be appreciated as a positive experience. For instance, Foxbot will reply to users with statements such as “Even if I only talk to you for a few minutes, it still makes my day.”
- Self-regulation for the persistent patience and continual availability afforded to users from a chatbot platform. This is further expanded in the way Foxbot monitors user interaction to see how the conversation is progressing, and extending it to deliver more content if needed.
- Social intelligence for the dialogue programmed into the chatbot communication algorithms, which have been informed by both prospective users and field experts.
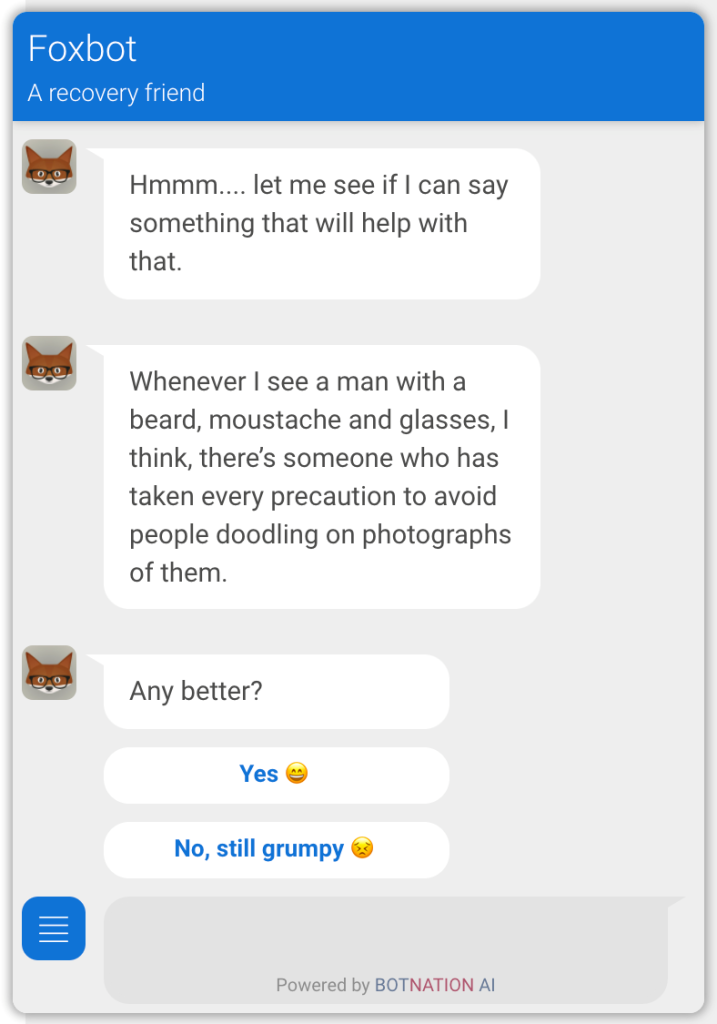
- Humor to offer a competing emotion that can be channeled to counteract low mood (see Figure 2).
- Creativity in recognition of the innovative use of the chatbot platform in delivering the PRIs.
Positive Recovery Interventions
The PRIs were adapted from a program of work currently under development called positive addiction recovery therapy (PART), which is in its preparatory stage and being delivered in small group settings. The aim of PART is to set the precedent that addicts in recovery can function better than they did prior to addiction.
PART uses an integrative approach, combining positive psychology with proven recovery principles to promote prorecovery thoughts and behavior to increase levels of happiness, well-being, and life satisfaction above those seen nationally in general populations. The results of a previous research project (Ogilvie & Carson, 2021) showed that positive interventions (e.g., mutual-support programs) were instrumental in raising the well-being of recovering alcoholics beyond that reported at a national level for the year 2019, where well-being generally declined because of the COVID-19 pandemic. The participants in the study reported that engaging in an activity that had a positive impact on their recovery increased their level of well-being, which protected them from relapse (Ogilvie & Carson, 2021). In deference to this, the PRIs selected for Foxbot are cognizant of the common challenges reported by people in recovery that contribute to or heighten the risk of relapse; for example, being triggered, having a craving, being in a bad mood, or needing to be grounded via a reality check (Melemis, 2015).
The PRIs were designed to actively face what users are experiencing in a bid to encourage perspective and help minimize the immediate risk to recovery. For instance, if individuals chatting to Foxbot indicate they are in a bad mood, Foxbot becomes a comedian and makes several attempts to lighten the mood by using humor, telling jokes, or presenting a humorous image (see Figure 2). In positive psychology humor has been linked to improved well-being (Niemiec, 2018), and it has been recognized for its therapeutic value in psychotherapy (Gonot-Schoupinsky et al., 2020).
Should users tell Foxbot they are having a craving, Foxbot explains the craving as a process that will pass, using positive mental imagery to show a wave rising, reaching its peak, and disappearing to the shore by means of explanation. The use of imagery has been shown to be effective in interrupting unhelpful thought processes (Pile et al., 2021). To complete this PRI, gamification is used to get users to detach from their cravings by engaging in an entertaining activity. Foxbot becomes a playmate and challenges users to beat a high score in a game of “join the dots.” Similarly, if users report being triggered they are reassured by Foxbot—a caring friend now—that facing challenges in recovery is normal and a reflection of something upsetting happening, not of a failing recovery. This is followed with an animated breathing exercise to reduce the physical reaction to the trigger and help stabilize the immediate distress being experienced.
Complacency and loss of self-focus heighten the risk of relapse, and can happen when those who have been in recovery for a sustained period believe they should be past their addiction, or perhaps feel they can no longer justify spending time on something that has already taken so much from their lives (Melemis, 2015). A reality check PRI attempts to readdress this complacency by offering a stark reminder and relatable example to users of what their addicted lives entailed. This is intended to reframe the thinking bias that is downplaying the severity of addiction. For example, Foxbot will select a response from a collection of statements such as “Dear alcohol, we had a deal where you would make me funnier, smarter, and more popular. I saw the video—you lied.” Furthermore, by reminding users that those in active addiction experience common consequences, the significance of understanding and empathy in recovery connection is reinforced (DiClemente, 2018).
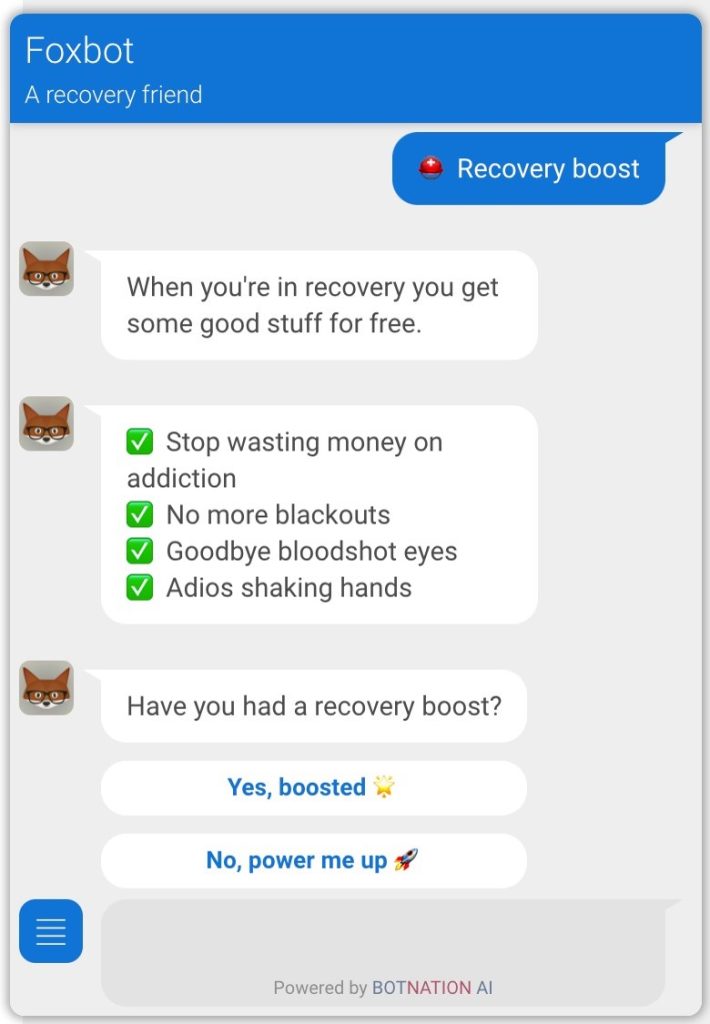
As befits the notion of positive intervention, users can opt to give themselves a recovery boost (see Figure 3). This PRI is intended to remind individuals of the benefits that have been acquired by virtue of choosing a recovery lifestyle (e.g., no more hangovers, no more shaking hands, and/or money saved is no longer feeding addiction). This is intended to promote gratitude for having chosen a recovery lifestyle and remind users of the freedom gained from no longer being in active addiction.
Discussion
Foxbot does not provide interventions with therapeutic depth for long-term problem resolution, but rather short-term and engaging interventions to mitigate the immediate risk of relapse. The PRIs delivered have been designed to be on the go, meaning that once users have sight of them through conversing with Foxbot, they can be applied by independently and, if required, without the chatbot. For instance, individuals can recall the positive mental image of the craving passing, remember one of the jokes that made them laugh when they were in a low mood, or give themselves a reality check when they sense that complacency is featuring in their recovery. Furthermore, in learning from previous chatbot implementations, the PRI design was informed by prospective users and field experts to provide valuable insight into what would be engaging and effective for the target user base (Janssen et al., 2021).
A challenge to developing solutions in areas subject to rapid technological advancement is the ability to gather evidence to demonstrate their efficacy. In health care this is problematic for longitudinal evaluation, as the technology can move quicker than the necessary window for study. In some cases, this has meant researchers have found that a chatbot solution has been decommissioned before a follow-up study can be conducted (Vaidyam et al., 2019). The basis for developing Foxbot was to afford support to addicts in recovery at the point of need. In reverence to this, Foxbot will not be decommissioned while usage statistics show active use—doing so would undermine the fundamental principle of the implementation. Subsequently, it is anticipated that sufficient time will be available for thorough study to gather evidence on the efficacy of using chatbots in this way. This piece of work has been scheduled along with plans for future enhancements.
Planned future enhancements include expanding Foxbot’s knowledge base to reduce the likelihood of repeat conversation. Currently this is controlled through random selection, which also enables protracted conversation when instigated by users. Going forward this process will be optimized by AI, when the chatbot will determine what content has been least used and therefore ready to be recycled. The present implementation approach uses branching logic, which offers more control over the user experience and is less error prone in so far as it can be programmed to behave in accord with the character of the chatbot. For instance, emphatic responses, or statements relaying gratitude, can reliably be presented to users when considered appropriate in the conversation (Adamopoulou & Moussiades, 2020). A technical review of the chatbot functionality will be conducted to see where AI capability can be better utilized with the decision-based logic to offer a more genuine conversational experience (Abd-alrazaq et al., 2019).
New PRIs will be added to Foxbot over time, offering end users an extended toolkit for their recovery. This will be influenced by data gathered and analysed by the AI engine on the historical conversations that have taken place. This analysis will provide insight into how Foxbot is being used, essentially empowering the chatbot to learn about addiction recovery from those using it. The output from this will allow Foxbot to engage in a process of self-improvement for future system enhancements.
In summary, chatbots have yet to make a notable impact in the addictions field, being an underrepresented area of study in comparison to other areas of mental health and health care (Ogilvie et al., 2021; Vaidyam et al., 2019). Given the intended audience, chatbots in addiction recovery are well placed to provide support to people who may be reticent to engage with alternate channels. They are available at the point of need when other support options may not be accessible, offering an immediate and focused solution for end users. Through their AI capability they can learn from recovering addicts to achieve a refined level of interaction that is not seen with other health care solutions. This comes with a note of caution however: as a chatbot solution moves away from decision-based logic toward the more authentic and human-like discourse accomplished through the increased use of AI, a greater responsibility is therefore placed on the system stakeholders to closely monitor usage to ensure that the system learns and behaves in an ethically sound way.
References
- Abd-Alrazaq, A. A., Alajlani, M., Alalwan, A. A., Bewick, B. M., Gardner, P., & Househ, M. (2019). An overview of the features of chatbots in mental health: A scoping review. International Journal of Medical Informatics, 132, 103978.
- Adamopoulou, E., & Moussiades, L. (2020). Chatbots: History, technology, and applications. Machine Learning with Applications, 2, 100006.
- Baumeister, R. F., & Nadal, A. C. (2017). Addiction: Motivation, action control, and habits of pleasure. Motivation Science, 3(3), 179–95.
- British National Health Service (NHS). (2021). NHS app. Retrieved from NHS https://www.nhs.uk/nhs-app/
- Calvo, R. A., & Peters, D. (2017). Positive computing: Technology for well-being and human potential. Cambridge, MA: MIT Press.
- DiClemente, C. C. (2018). Addiction and change: How addictions develop and addicted people recover (2nd ed.). New York, NY: Guilford Press.
- Elena-Bucea, A., Cruz-Jesus, F., Oliveira, T., & Coelho, P. S. (2021). Assessing the role of age, education, gender, and income on the digital divide: Evidence for the European Union. Information Systems Frontiers, 21(4), 1007–21.
- European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). (2021). European drug report: Trends and developments. Retrieved from https://www.emcdda.europa.eu/system/files/publications/13838/TDAT21001ENN.pdf
- Gonot-Schoupinsky, F. N., Garip, G., & Sheffield, D. (2020). Laughter and humour for personal development: A systematic scoping review of the evidence. European Journal of Integrative Medicine, 37(2), 101144.
- Janssen, A. H. A., Grützner, L., & Breitner, M. H. (2021). Why do chatbots fail? A critical success factors analysis. Presented at the 42nd International Conference on Information Systems, December 12–15, 2021 in Austin, Texas. Retrieved from https://aisel.aisnet.org/icis2021/hci_robot/hci_robot/6/
- Matthews, S., Dwyer, R., & Snoek, A. (2017). Stigma and self-stigma in addiction. Journal of Bioethical Inquiry, 14(2), 275–86.
- Melemis, S. M. (2015). Relapse prevention and the five rules of recovery. Yale Journal of Biology and Medicine, 88(3), 325–32.
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2022). Alcohol facts and statistics. Retrieved from https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
- Niemiec, R. M. (2018). Character strengths interventions: A field guide for practitioners. Newburyport, MA: Hogrefe.
- Ogilvie, L., & Carson, J. (2021). The feeling’s mutual. Drink and Drugs News. Retrieved from https://www.drinkanddrugsnews.com/the-feelings-mutual/
- Ogilvie, L., Prescott, J., & Carson, J. (2021). The use of chatbots as supportive agents for people seeking help for drug and alcohol addiction: A systematic review. Journal of Medical Internet Research. Retrieved from https://s3.ca-central-1.amazonaws.com/assets.jmir.org/assets/preprints/preprint-31227-submitted.pdf
- Pile, V., Williamson, G., Saunders, A., Holmes, E. A., & Lau, J. Y. F. (2021). Harnessing emotional mental imagery to reduce anxiety and depression in young people: An integrative review of progress and promise. Lancet Psychiatry, 8(9), 836–52.
- Public Health England. (2020). Adult substance misuse treatment statistics 2019 to 2020: Report. Retrieved from https://www.gov.uk/government/statistics/substance-misuse-treatment-for-adults-statistics-2019-to-2020/adult-substance-misuse-treatment-statistics-2019-to-2020-report
- Turner, S., Mota, N., Bolton, J., & Sareen, J. (2018). Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and Anxiety, 35(9), 851–60.
- Vaidyam, A. N., Wisniewski, H., Halamka, J. D., Kashavan, M. S., & Torous, J. B. (2019). Chatbots and conversational agents in mental health: A review of the psychiatric landscape. Canadian Journal of Psychiatry, 64(7), 456–64.
- van Gemert-Pijnen, L., Kelders, S. M., Kip, H., & Sanderman, R. (2018). eHealth research, theory, and development: A multidisciplinary approach. London: Routledge.
- VIA Institute on Character. (n.d.). The twenty-four character strengths. Retrieved from https://www.viacharacter.org/character-strengths
About Me
Lisa Ogilvie, MSc, is a doctoral student at the University of Bolton where she is developing a program of work called positive addiction recovery therapy (PART). She graduated with distinction in her MSc in counseling and positive psychology and now specializes in the application of positive psychology in the field of addiction recovery. Ogilvie is also interested in how technology can be used to improve the well-being of people in addiction recovery. In addition to working on her PhD, she is a qualified counselor who volunteers for an addiction treatment service.
Jerome Carson, PhD, is a professor of psychology at the University of Bolton. He is interested in the field of alcohol addiction and recovery from a lived experience perspective, though interestingly much of his research has been in the field of mental health recovery. Dr. Carson researches the area of positive psychology and autoethnography, and is also a qualified clinical psychologist.
Julie Prescott, PhD, is the program lead for the undergraduate psychology, psychotherapy, and counseling program at the University of Bolton. She is a senior fellow of the Higher Education Academy, a chartered psychologist, associate fellow of the British Psychological Society, and holds APA membership. Dr. Prescott’s current research area focuses on technology and health/mental health, with a particular interest in young people and online counseling as well as how people gain support and use online technologies for health/mental health support. She is on the editorial board for JMIR Mental Health, a sister journal to the leading health and technology journal JMIR.












 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.