Share
The national focus on improving access to treatment for opioid use disorder (OUD) extends beyond providers who can prescribe buprenorphine. Pharmacy-level barriers exist for patients seeking to fill buprenorphine prescriptions at traditional retail pharmacies that may negatively impact access to the medication itself, and consequently result in less than optimal treatment and health outcomes. Patients cannot be adherent to their treatment regimen without their medication, and when nonadherent, the risk of relapse significantly increases (Bell & Strang, 2020, Lander et al., 2020). Programs designed to improve the likelihood that patients diagnosed with OUD fill their buprenorphine prescriptions, and therefore support the likelihood of patients taking their medication, have meaningful implications for both patients and treatment providers.
One advantage of utilizing buprenorphine to treat OUD is that patients are not required to report to a designated program for observed daily dosing. However, with the ability to independently dose comes added patient responsibility to travel to a pharmacy to fill buprenorphine prescriptions in addition to overcoming barriers that may exist to attend scheduled treatment appointments. Buprenorphine enables physicians to treat patients with OUD in a similar manner to other chronic disease states and helps to support a change in perspective toward OUD from both the medical community and society. Yet, patients diagnosed with OUD are still not always viewed in the same respect as those with diabetes, heart disease, asthma, or other chronic conditions (Ling et al., 2012). Although approximately 90 percent of Americans live within five miles of a retail pharmacy, proximity to medication does not necessarily equate to access to medication (Frederick, 2015). Specifically, OUD patients are commonly subject to judgment when seeking to fill their prescriptions and face uncertainty around whether these retail pharmacies even stock and dispense buprenorphine.
Furthermore, when it comes to filling buprenorphine prescriptions, pharmacies report experiencing ambiguity navigating what the Drug Enforcement Administration (DEA) regulations are, inability to meet patient demand, wholesaler limitations, stigma from pharmacy staff, and fear of patient diversion. These hesitations may result in pharmacists limiting quantity, capping patients served, or shying away from stocking and dispensing buprenorphine altogether (Haelle, 2019). Ultimately, these create additional pharmacy-level barriers for patients to navigate on their road to recovery.
The American Pharmacists Association advocates for the essential role that pharmacists play in addiction treatment, specifically in helping to positively impact opioid misuse and diversion, yet many times pharmacists are an underutilized resource in the care of those diagnosed with OUD (Thakur et al., 2019). Literature supports that care coordination and collaboration between pharmacists and prescribers improves patient care and health outcomes. For example, integration of onsite pharmacies within community mental health centers revealed higher medication adherence rates as well as lower hospitalization and emergency department use for participating patients, translating into reductions in health care costs (Wright et al., 2016).
Additionally, studying a physician-pharmacist collaborative practice model designed to optimize patient care for buprenorphine-maintained, opioid-dependent patients demonstrated meaningfully high retention rates at six and twelve months, as well as high medication adherence and low opioid use amongst patients in the program (DiPaula & Menachery, 2015). Further, a recent study demonstrated high rates of six-month patient retention and visit adherence when community pharmacists trained on OUD and features of buprenorphine treatment helped manage care for patients with the diagnosis (Wu et al., 2021). This study also concluded that buprenorphine treatment visits located at the same place where medication is provided is extremely useful and convenient.
Strategies that target treatment retention, relapse prevention, and harm reduction are common goals amongst many office-based opioid treatment programs. Longer retention in treatment for OUD has been associated with favorable patient outcomes, but retention can be challenging with many patients discontinuing treatment prematurely within a few weeks or months after initiation (Weiss et al., 2015; Williams et al., 2018). Patients seeking a buprenorphine medication-assisted treatment (MAT) program must overcome the initial challenge of finding a treatment provider to begin their recovery journey, then continue to attend scheduled office visits and remain active and engaged in their treatment regimen, which encompasses consistent filling of prescribed buprenorphine at retail pharmacies.
Medication adherence is a key component of the efficacy of MAT, as patients who are nonadherent to their buprenorphine treatment plan are at significantly greater risk for poor outcomes (Ronquest et al., 2018). Simplifying the traditionally two-step process of obtaining a buprenorphine prescription from a provider and then filling the medication at a retail pharmacy to be inclusive at the time of a single treatment visit provides patients with convenient, fast, and judgment-free access to their medication without worry or stress. The coordination of buprenorphine medication pickup at the time of patients’ treatment visit alleviates the need for patients to seek a pharmacy to fill their prescriptions, supports medication adherence as patients leave treatment with their buprenorphine in hand, and acknowledges that making it to treatment means leaving with medication, which may be a motivating factor for patients to attend scheduled treatment appointments.
A recent study by these authors (i.e., Khan, Khan, and Kolb) published in the Journal of Substance Abuse Treatment details a pre-post retrospective chart review that was performed to evaluate the potential positive impact on patient retention and health outcomes when prescribing and pharmacy services are integrated for patients prescribed buprenorphine for the treatment of OUD (Khan et al., 2021). The patients studied were enrolled in a clinic-based, managed pharmacy program that was established to align medication access with written prescriptions and create a direct, trusted relationship between prescribers and pharmacists, allowing for a continuum of care. Patients in the program had their prescriptions filled by a pharmacy that coordinated medication delivery with the clinic’s appointment schedule such that a pharmacy representative within the office gave each patient their prescribed buprenorphine at the conclusion of their clinic visit. The pharmacist is experienced in caring for patients who have been prescribed buprenorphine and is complemented by a compliance leader with regulatory experience. The pharmacist checks the prescription drug monitoring program and reviews drug test results to ensure buprenorphine is present and to identify any unexpected substance use for each patient, raising irregularities prior to filling the buprenorphine. Additionally, the pharmacy offers lifesaving naloxone to each patient in the program. Other key features of the program include a pharmacy liaison present during clinic office hours to deliver medication to the patients, facilitate patient engagement, and manage communication and coordination between clinic schedule and medication delivery.
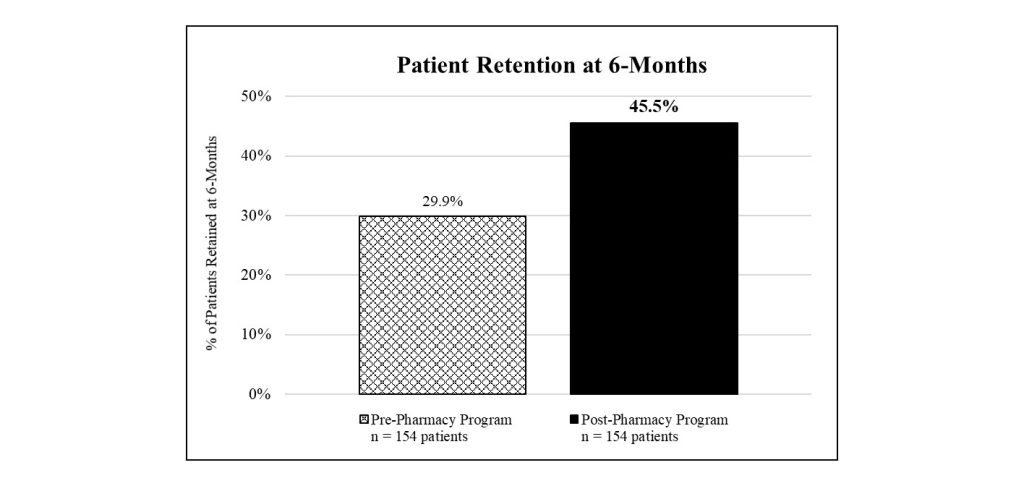
The study revealed that medication adherence, illicit and nonprescribed drug use, drug-related emergency department utilization, and retention in care all significantly improved following implementation of the clinic-based pharmacy services when compared with patients treated at the same clinic filling their buprenorphine prescriptions at retail pharmacies. Furthermore, patients expressed high satisfaction with the program that alleviated the need for them to fill their buprenorphine prescriptions at pharmacies, as captured through a voluntary and anonymous survey. Patients were more likely to make their scheduled treatment appointments when the pharmacy delivered their buprenorphine medication in coordination with their visit and demonstrated a 52.2 percent higher retention rate at six months as compared with how patients were getting their medication prior (see Figure 1).
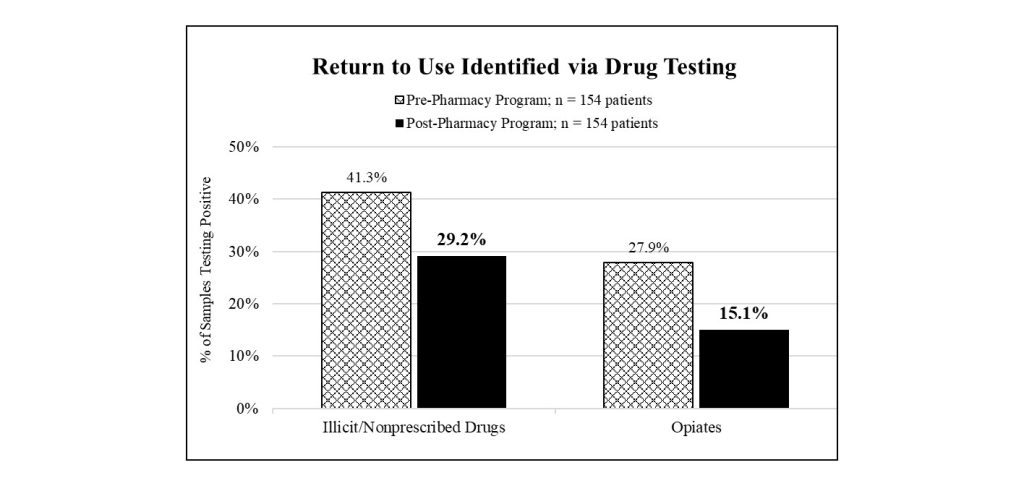
Additionally, the study reviewed lab testing results obtained from observed urine drug screens performed at each office visit and testing for buprenorphine adherence and illicit/nonprescribed drug use (e.g., amphetamines, cocaine, methadone, opiates). The urine drug screens demonstrated a higher rate of medication adherence and significantly lower rate of illicit/nonprescribed drug use for patients enrolled in the pharmacy program. The buprenorphine positivity rate was 92.5 percent for patients in the pharmacy program, as compared with 85.8 percent observed for patients prior. Moreover, 29.2 percent of samples tested from patients in the program indicated use of illicit/nonprescribed drugs as compared with 41.3 percent observed for patients prior. Specifically, 45.9 percent fewer samples tested from patients in the program revealed opiate use, with an opiate positivity rate of 15.1 percent for patients in the program and 27.9 percent for patients prior (see Figure 2).
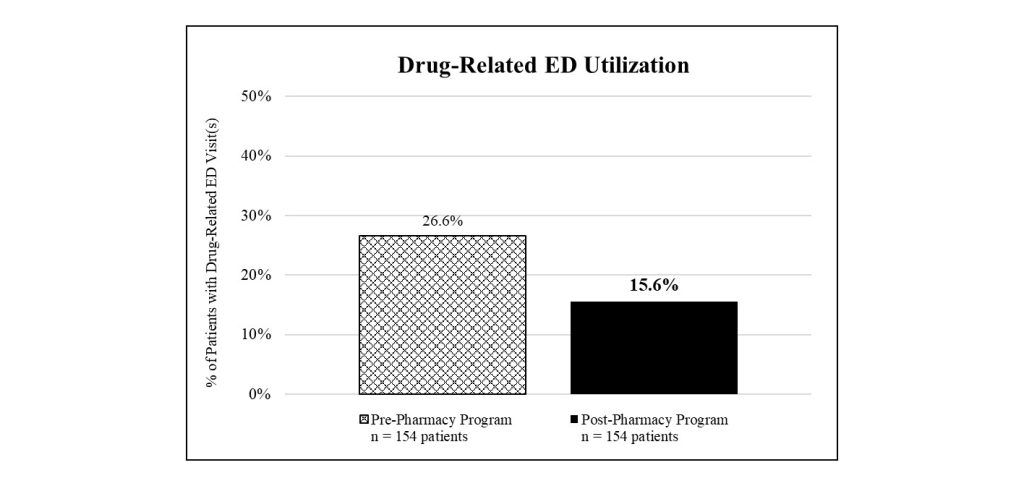
Further, the study documented many instances of drug-related emergency department utilizations per patient, including visits due to overdose, abscess from injection site, injury while on drugs, sickness from withdrawal, fear or sickness while on drugs, and drug-seeking behavior and suicide attempts where indication of illicit drug use or misuse of prescription medication was noted. Findings indicated that 41.4 percent fewer patients in the program utilized the emergency department for one or more of these reasons as compared with patients prior. Specifically, 15.6 percent of patients in the pharmacy program sought the emergency department for drug-related reasons, corresponding to forty-three visits, as compared with 26.6 percent of patients prior, corresponding to eighty-one visits (see Figure 3).
Today, this clinic-based pharmacy program serves thousands of patients spanning eleven states and reports similar findings of high retention, adherence, and satisfaction as new clinics incorporate the pharmacy program into their practice as an extension of treatment services. An ongoing patient experience survey has captured the feedback of over 1,100 patients at twenty-nine office-based opioid treatment clinics receiving their buprenorphine at their visit through the program. Survey results reveal consistently high patient satisfaction, provide meaningful insights into the impact of the program, and help to put numbers behind the pharmacy-level barriers that exist without the program.
Transportation challenges or undue time spent obtaining medication prior to the program was noted by 77 percent of respondents, followed by experiencing stigma and shame at retail pharmacies noted by 55 percent of respondents, and pharmacies not reliably stocking their medication noted by 34 percent of respondents. The survey found that 98 percent of patients agreed the pharmacy liaison treats them with respect and cares about their well-being. Additionally, 93 percent of patients agreed that receiving buprenorphine at the time of their treatment visit makes them more likely to attend appointments and stick with their treatment plan. The survey produced a net promoter score of eighty-four, signifying that the patients surveyed are highly satisfied with the pharmacy program experience and service level.
Furthermore, the survey also includes an open-ended question that asks patients to provide a sentence or two regarding how receiving their medication at the clinic versus at a retail pharmacy has impacted their recovery. Common themes mentioned in the patient responses were that the pharmacy program is more convenient, more private, easier, faster, stress free, judgment free, and that it supported their recovery engagement and success. Select quotes from this survey question are highlighted and shed valuable light on how removing one key barrier to access makes a substantial difference:
- “It’s a relief I can do everything while I’m here, and I don’t have to worry about the pharmacy having my meds or people judging me.”
- “It helps me feel normal again. Something I haven’t had in a while.”
- “Rather than waiting until I go to the pharmacy, I received medication at the doctor’s office. Less time in between doctor and meds means less time to make bad decisions.”
- “By receiving my meds at my doctor’s office, it makes me feel better about myself and no one knows what I have going on in my life. I feel like everyone else.”
- “It’s helped keep me from running into people that could affect my sobriety at the pharmacy.”
- “It’s made it less stressful. No stigma attached to Suboxone by Cordant.”
Removing harmful barriers to treatment is a top priority in the addiction space, making programs aimed at improving patient care—such as alleviating the need to fill prescriptions at local pharmacies through clinic-based buprenorphine provision—extremely valuable. Although the study was performed at a single office-based opioid treatment clinic and has limitations, the positive outcomes serve as an indicator that broader implementation of this clinic-based managed pharmacy program may have significant benefit for office-based opioid treatment clinics treating similar patients. The study can further support the value of care coordination between prescribers and pharmacists to positively impact patient outcomes.
More research is needed in the addiction treatment space to identify opportunities to improve care, including additional studies on this important and not well-understood topic, and to determine causality and generalizability of results. Providing patients with confidence and confidentiality in receiving their medication when they need it and at the same location as their treatment appointments addresses pharmacy-level barriers that exist and supports patient success in the recovery journey.
References
- Bell, J., & Strang, J. (2020). Medication treatment of opioid use disorder. Biological Psychiatry, 87(1), 82–8.
- DiPaula, B. A., & Menachery, E. (2015). Physician-pharmacist collaborative care model for buprenorphine-maintained opioid-dependent patients. Journal of the American Pharmacists Association, 55(2), 187–92.
- Frederick, J. (2015). By the numbers: How community pharmacists measure up. Drug Store News. Retrieved from
- Haelle, T. (2019). Pharmacist stigma a barrier to rural buprenorphine access. Retrieved from https://www.mdedge.com/psychiatry/article/205251/addiction-medicine/pharmacist-stigma-barrier-rural-buprenorphine-access
- Khan, A., Khan, Q., & Kolb, E. (2021). Supportive alternate site provision of buprenorphine: Overcoming barriers and improving patient outcomes. Journal of Substance Abuse Treatment, 123, 108256.
- Lander, L. R., Zheng, W., Hustead, J. D., Mahoney III, J. J., Berry, J. H., Marshalek, P., & Winstanley, E. L. (2020). Long-term treatment retention in West Virginia’s comprehensive opioid addiction treatment (COAT) program. Journal of the Neurological Sciences, 411, 116712.
- Ling, W., Mooney, L., & Torrington, M. (2012). Buprenorphine for opioid addiction. Pain Management, 2(4), 345–50.
- Ronquest, N. A., Wilson, T. M., Montejano, L. B., Nadipelli, V. R., & Wollschlaeger, B. A. (2018). Relationship between buprenorphine adherence and relapse, health care utilization, and costs in privately and publicly insured patients with opioid use disorder. Substance Abuse and Rehabilitation, 9, 59–78.
- Thakur, T., Frey, M., & Chewning, B. (2019). Pharmacist services in the opioid crisis: Current practices and scope in the United States. Pharmacy, 7(2), 60.
- Weiss, R. D., Potter, J. S., Griffin, M. L., Provost, S. E., Fitzmaurice, G. D., McDermott, K. A., Srisarajivakul, E. N., Dodd, D. R., Dreifuss, J. A., McHugh, R. K., & Carroll, K. M. (2015). Long-term outcomes from the National Drug Abuse Treatment Clinical Trials Network prescription opioid addiction treatment study. Drug and Alcohol Dependence, 150, 112–9.
- Williams, A. R., Nunes, E. V., Bisaga, A., Pincus, H. A., Johnson, K. A., Campbell, A. N., Remien, R. H., Crystal, S., Friedmann, P. D., Levin, F. R., & Olfson, M. (2018). Developing an opioid use disorder treatment cascade: A review of quality measures. Journal of Substance Abuse Treatment, 91, 57–68.
- Wright, W. A., Gorman, J. M., Odorzynski, M., Peterson, M. J., & Clayton, C. (2016). Integrated pharmacies at community mental health centers: Medication adherence and outcomes. Journal of Managed Care & Specialty Pharmacy, 22(11), 1330–6.
- Wu, L.-T., John, W. S., Ghitza, U. E., Wahle, A., Matthews, A. G., Lewis, M., Hart, B., Hubbard, Z., Bowlby, L. A., Greenblatt, L. A., & Mannelli, P. (2021). Buprenorphine physician-pharmacist collaboration in the management of patients with opioid use disorder: Results from a multisite study of the National Drug Abuse Treatment Clinical Trials Network. Addiction, 116(7), 1805–16.
Editor’s Note: This article was adapted from an article by the same authors previously published in the Journal of Substance Abuse Treatment (JSAT). This article has been adapted as part of Counselor’s memorandum of agreement with JSAT. The following citation provides the original source of the article:
- Khan, A., Khan, Q., & Kolb, E. (2021). Khan, A., Khan, Q., & Kolb, E. (2021). Supportive alternate site provision of buprenorphine: Overcoming barriers and improving patient outcomes. Journal of Substance Abuse Treatment, 123, 108256.
About Me
Asif Khan, MD, FASAM, FACP, is an assistant professor at the University of Washington. He is a member of the Pierce County Opioid Task Force and the State of Washington Criminal Justice Opioid Work Group. Dr. Khan also serves as vice chair of the Washington State Association of Treatment of Opioid Dependence and is a member of the Washington Association of Alcoholism and Addiction Programs.
Qudsia Khan, MD, is a board-certified internal medicine physician and completed her residency at University of Illinois/Mercy Hospital and Medical Center. She currently serves as chief medical officer at Northwest Integrated Health and holds a faculty appointment as a clinical assistant professor at Pacific Northwest University. Dr. Khan was a member of Provider Integration Panel with Pierce County ACH to improve collaboration across the county to enhance regional cooperation. She is the medical director of STR Hub and Spoke grant for Pierce County to reduce barriers to obtain treatment for opioid use disorder.
Elizabeth Kolb, MS, received her bachelor’s of science in biochemistry from Adelphi University and completed her master’s degree in forensic science at John Jay College of Criminal Justice. She is the senior director of corporate development and strategy at Cordant Health Solutions.












 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.