Share
As a clinician, working with young adults (ages eighteen to twenty-nine) can pose many challenges. Overall, young adults exhibit the highest rates of cannabis use (19 percent), alcohol use (59.6 percent), binge drinking (37.9 percent), and illicit drug use (21.5 percent) compared to adolescents and older adults (SAMHSA, 2014). In addition to having the highest prevalence rates of substance use, young adults represent a large proportion of treatment admissions in the United States. In 2013, over 22 million people needed treatment for alcohol or drug use problems and, among treatment admissions, 22 percent of individuals received some form of residential care. A large proportion (34 percent) of these individuals receiving treatment were young adults (SAMHSA, 2013).
Residential care can include a wide variety of treatment options from basic supportive therapy (e.g., Twelve Step facilitation, group therapy) to manualized interventions. Recently, mindfulness-based interventions have become a popular treatment for a multitude of psychiatric problems such as depression, anxiety, eating disorders, and, more recently, substance use disorders (Brewer, Bowen, Smith, Marlatt, & Potenza, 2010; Bowen, Witkiewitz, Chawla, & Grow, 2011; Brewer, Elwafi, & Davis, 2013; Li, Howard, Garland, McGovern, & Lazar, 2017; Zgierska et al., 2008). Specifically, mindfulness-based relapse prevention (MBRP) was developed to target negative thought processes such as rumination and craving, which both play significant roles in substance use relapse (Witkiewitz, Bowen, Douglas, & Hsu, 2013). However, to date no study has investigated how MBRP may be a useful intervention for young adults. The effectiveness and mechanisms used in mindfulness interventions for substance use disorders will be reviewed below in addition to exploring how mindfulness interventions improve substance use, stress, and craving during and following treatment completion. Further, an overview of the current study will be presented along with some potential clinical implications.
What is Mindfulness?
How one defines mindfulness has been a topic of debate for years. Often when we ask our clients (or even our colleagues) what mindfulness is, we might receive a response such as “it means not having any thoughts” or “being relaxed and calm.” While this might be the way mindfulness is viewed to the general public, it certainly is not how early adopters of mindfulness would describe it. Mindfulness is a meditation practice dating back nearly 2,500 years. Buddhist thought would assert that an individual’s ability to ruminate about the past or grasp onto an unattainable future is not being fully present which can alter one’s perception of reality. Today in Western culture, the definition of mindfulness has gone through many iterations. Generally, most psychologists or mindfulness practitioners would agree that mindfulness is being more aware of the present moment; it is a practice that is deliberate, requires practice outside of sitting meditation, and allows for the observation of both cognitive and sensory experiences. This present moment awareness can take the form of paying attention to emotional reactions, mental images or memories, bodily sensations, or any number of experiences one might be having. Further, one can think of mindfulness as maintaining an attitude of openness or acceptance towards one’s experience. In fact, the way most individuals view mindfulness (e.g., no thoughts) is precisely what mindfulness is not. The way I like to describe mindfulness to my clients is “Mindfulness is the deliberate act of bringing our attention back to the present moment, whether that be the breath, thoughts, emotions, etc., when our mind begins to wander.” In the box below, we present one of the most common meditations used in nearly every curriculum: mindfulness of the breath. Give it a go with a colleague or family member.
Mindfulness Interventions for Substance Use Problems
Over the past decade mindfulness has become a hot topic. In fact, one could argue that mindfulness, both practice and research, is one of the fastest growing areas in psychology. Beginning with mindfulness-based stress reduction (MBSR), which was largely based on Buddhist contemplative practices, numerous interventions have been developed to target a range of psychiatric and medical conditions. For example, mindfulness-based cognitive therapy was developed for depression, mindfulness-based eating awareness training (MB-EAT) for binge eating, mindfulness training for smokers (MTS), and mindfulness-based relapse prevention (MBRP) for substance use disorders. However, despite the popularity of investigating mindfulness interventions in the scientific arena, less than 9 percent of studies assessing mindfulness interventions have used a control group (e.g., comparing mindfulness interventions to some other form of treatment; Baer, 2003; Bishop et al., 2004; Goldberg et al., 2018). This is alarming given the number of randomized controlled trials—the gold standard for clinical trial studies—increased from eleven between 2004 and 2006 to 216 between 2013 and 2015.
Studies of clinical populations have shown that clients entering substance use treatment report heightened levels of stress and an inability to adaptively cope with acute stressors (See Sinha, 2007 for review). MBRP was developed to target negative thought processes such as rumination and craving, which both play significant roles in substance use relapse (Witkiewitz et al., 2013). Staying true to the principles of mindfulness-based practices, MBRP aims to increase a patient’s ability to tolerate problematic cognitive, as well as physiological, experiences by helping patients to remain present focused which is typically achieved through meditative practice (Bowen et al., 2009). This means during treatment participants are taught to “respond” to situations that may trigger use or rumination through present-moment focus rather than acting or reacting in a habitual manner (Witkiewitz & Bowen, 2010). MBRP adds an interesting aspect to mindfulness-based treatments in that the intention is to enhance awareness of their internal and external triggers (Bowen et al., 2011). That is, MBRP adds an element of traditional cognitive behavioral exercises that aid in identifying high risk situations while creating alternative responses and coping strategies to respond to those triggers (Witkiewitz & Bowen, 2010). These skills are vital as both impulsivity and rumination are significant hindrances to posttreatment success.
Research on the effectiveness of MBRP and other mindfulness interventions for substance use disorders has grown substantially over the last five years. In a recent meta-analysis, Li and colleagues (2017) found an overall effect of mindfulness-based treatments (no specificity) of d = -.33 for any substance. This means we can expect 58 percent of individuals in the intervention group (e.g., mindfulness-based interventions) to be below the mean level of substance use of individuals in the control group. Specific to illicit drug use, results were replicated with a Cohen’s d of -.51 for opiate use. One of the strongest effects of mindfulness-based interventions was on stress with an overall effect size of d = -1.21. That is, nearly 88 percent of individuals in the intervention group will be below the mean stress scores of the control group. Specific to MBRP, Bowen et al. (2009) randomly assigned participants (n = 168) to MBRP versus standard care. Individuals assigned to MBRP had significantly fewer days of alcohol and drug use two months following the intervention. Further, individuals assigned to MBRP showed significant reductions in craving and acceptance and a large majority (58 percent) reported continued practice four months after completion of treatment. The first evaluation of MBRP as a stand-alone treatment by Brewer et al. (2009) randomly assigned participants (n = 36) who had alcohol or cocaine use disorders to MBRP or group cognitive behavioral therapy. At follow-up, no significant group differences were found for substance use outcomes, but those assigned to mindfulness training had significantly better reductions in physiological and psychological stress reactivity following a stress provocation lab task. Most recently, Witkiewitz et al. (2014) investigated the effect of MBRP versus relapse prevention among women offenders in residential substance use treatment. Participants (N = 105) were randomly assigned to receive eight sessions of MBRP (n = 55) or RP (n = 50). Results indicated at the fifteen-week follow-up that individuals assigned to MBRP showed significantly fewer days of drug and alcohol use (d = .36 – .45), and significantly fewer legal problems (d = 1.18) compared to individuals assigned to relapse prevention. Bowen et al. (2014) randomly assigned adults assigned to MBRP (n = 103), relapse prevention (n = 88), and treatment as usual (TAU; n = 95). Compared to TAU, individuals assigned to MBRP and relapse prevention showed a 54 percent decreased risk of relapse for drug use and a 59 percent decrease risk of relapse to heavy drinking. Thus, the efficacy for mindfulness-based interventions is strong, yet little is known in regards to how well mindfulness-based treatments, specifically MBRP, work for younger populations such as young adults.
Our Study
In the current study, we sought to understand if MBRP is a useful, viable, and appropriate treatment for young adults in residential substance use disorder treatment. Recruitment for the study began on September 1, 2015 and ended on November 15, 2016. To be included in the current study, participants had to be between the ages of eighteen and twenty-nine years old, be a current resident at the treatment center, have a substance use disorder (required for residential treatment), be proficient in the English language, and possess clear cognitive ability to understand and provide consent. Following consenting procedures, all participants underwent an initial baseline assessment. The baseline assessment took, on average, between forty and sixty minutes to complete. Each of the eligible and consented young adults completed a baseline assessment that evaluated various psychological, social, and behavioral domains. After consenting, participants were randomized to receive MBRP or TAU. All participants, regardless of group assignment received the treatment provided at the residential facility. However, those assigned to the experimental group received eight additional sessions of MBRP and those assigned to the control group attended eight additional self-help (e.g., Twelve Step, Alcoholics Anonymous, Narcotics Anonymous) sessions. All participants completed bimonthly (two per month) assessments for six months following the baseline assessment. Thus, during the treatment phase, participants completed two assessments: two weeks after baseline and at treatment completion, which was approximately four weeks after the baseline assessment and twelve assessments following treatment discharge. In the current study, we were interested in three main outcomes: days of substance use, perceived stress, and craving.
What Did We Find?
To give readers an idea of what our sample looked like, participants were, on average, twenty-five years old (SD = 2.7), primarily male (n = 52, 65 percent), and white (n = 73, 91.3 percent). The majority of participants were single (n= 48, 60 percent), not in college or university (n = 70, 87.5 percent) prior to entering the residential facility, on average participants had a high school degree (or equivalent; Mean years of education = 11.9 (SD = 1.6)), and were primarily unemployed (n = 52, 65 percent). When looking at salary (a crude measurement of socioeconomic status), the median salary was 5,500 USD per year. No significant differences were found between MBRP or TAU groups across all demographic variables. In terms of substance use, most participants (over 90 percent) were polysubstance users. On average, participants were 12.7 (SD 2.8) years old when they first used any substance.
The mo
st used substances were alcohol (past ninety-day Mean = 17.5 days), cannabis (past ninety-day Mean = 27.4 days), m
ethamp
hetamine (past ninety-day Mean = 19.1 days), and heroin (past ninety-day Mean = 14.3 days).
Looking at Figure 1, we can see that young adults assigned to the control 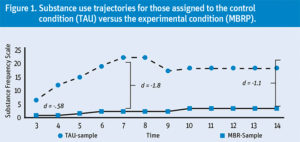 condition had steeper increases in substance use during the post-treatment phase compared to young adults assigned to MBRP. In fact, you might notice that the gap gets wider as we go out in time, indicating that the effects of MBRP seem to persist following treatment discharge.
condition had steeper increases in substance use during the post-treatment phase compared to young adults assigned to MBRP. In fact, you might notice that the gap gets wider as we go out in time, indicating that the effects of MBRP seem to persist following treatment discharge.
Further, looking at Figure 2, we can see that for craving, both control conditions and experimental have significant decreases in craving during the treatment phase. However, you may notice a stark increase in craving for young adults in the control condition immediately following tr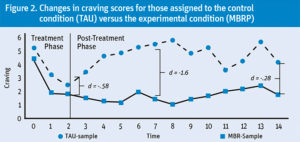 eatment discharge. Finally, looking at Figure 3, we see a similar pattern for stress. However, during the treatment phase stress reduces at similar rates for both groups. Yet the effect of MBRP on perceived stress persists during the posttreatment, as those assigned to MBRP maintain their post-treatment stress levels and those assigned to TAU have a slow and gradual increase in perceived stress. Finally, our results also indicated that stress was a significant mechanism linking MBRP to reduced substance use.
eatment discharge. Finally, looking at Figure 3, we see a similar pattern for stress. However, during the treatment phase stress reduces at similar rates for both groups. Yet the effect of MBRP on perceived stress persists during the posttreatment, as those assigned to MBRP maintain their post-treatment stress levels and those assigned to TAU have a slow and gradual increase in perceived stress. Finally, our results also indicated that stress was a significant mechanism linking MBRP to reduced substance use.
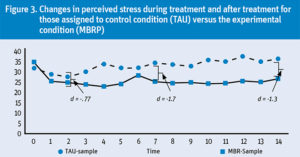
That is, those assigned to MBRP had lower stress scores during treatment, and these lower stress scores were associated with decreased substance use during the posttreatment phase.
Clinical Implications
Mindfulness is a Buddhist-based practice focused on one’s present state of awareness (Brown & Ryan, 2003). There has been a recent increase of interventions incorporating practices based on such beliefs. In fact, some researchers have suggested that mindfulness-based treatments for substance use may have significant advantages over traditional treatments (Brewer et al., 2013) in that they support patients’ ability to stay in touch with their experiences instead of avoiding or removing negative stimuli (Chiesa, Anselmi, & Serretti, 2014). The current study suggests that MBRP is a viable, acceptable, and useful intervention for young adults in residential treatment. In fact, we found that compared to those assigned to additional Twelve Step meetings, those receiving MRBP had better substance use, craving, and stress outcomes six months after initial engagement with treatment. We should also note that the current sample of young adults represents what the Institute of Medicine would consider a marginalized population. That is, the Institute of Medicine recently released a report on the health and well-being of emerging adults (Bonnie, Stroud, & Breiner, 2015) calling for a more comprehensive investigation of the risks, health, safety, and development of marginalized emerging adults, in particular. Marginalized emerging adults—those who have been involved in the child welfare system, criminal justice system, or have not attended some form of higher education—have high risk for mental and physical health problems, as well as substance use problems (McNiel, Binder, & Robinson, 2014; Traube, James, Zhang, & Landsverk, 2012; Walters et al., 2014; White, Labouvie, & Papadaratsakis, 2005). In fact, in a recent meta-analysis that our team completed, we investigated the effect of substance use treatment outcome studies in non-college settings for young adults (Davis, Smith, & Briley, 2017). We found larger treatment effects for studies that contained a higher proportion of participants currently in college or university. Results from this study indicate a need to understand, more fully, treatment effects among emerging adults outside of the college or university system.
In the current study, treatment fidelity was high and the clinicians had extensive training in mindfulness-based interventions. Thus, clinicians wishing to implement MRBP or similar protocol may need extensive training to see similar results. While this may appear to be a limitation—it implies that, with correct training and implementation, clinicians may see similar results. This would, however, include extensive supervision and, opens the door to future research on implementation and dissemination of MBRP in the context of treatment centers. In fact, recent research suggests that upwards of 33 percent of practitioners are, in general, familiar with and currently implementing mindfulness interventions for substance using populations (Edwards, Cohen, & Wupperman, 2016). However, only 7 percent are currently providing a research supported mindfulness interventions, indicating additional training and accessibility to mindfulness resources are needed.
One of the more important findings in the current study was the effects of MBRP on stress and the mediating role stress played in reducing substance use. Individuals assigned to MBRP had significantly lower stress scores during both the treatment phase and the posttreatment phase. In particular, when looking at the standardized effects, individuals assigned to MBRP had a 62 percent decrease in stress during the treatment phase and a 35 percent decrease in stress during the posttreatment phase. Li and colleagues (2017) reported that reductions in stress had the largest effect size across all studies assessing effectiveness of mindfulness interventions for substance use disorders. Specifically, they found a Cohen’s d of -1.12 for stress indicating a large effect of mindfulness-based interventions on stress.
It is well known that prolonged or repeated exposure to stress can increase one’s health risks (Cohen et al., 2002; Cohen, Janicki-Deverts, & Miller, 2007; McEwen, 1998). Given stress is one of the most well-known contributors to initiation and continuation of substance use (Shonkoff & Garner, 2012; Sinha, 2008), assessing how a treatment, mindfulness, targets reduction in stress is vital for understanding recovery processes. The stress response system consists of two major components: physiological stress response and psychological stress response. From a physiological perspective, stress response has been associated with a variety of neuroendocrine responses (e.g., cortisol production) and activation of neurological pathways associated with increased risk for drug use (Gordon, 2002). For example, in nonhuman primate studies, high-stress environments are associated with heightened corticotropin releasing factor (CRF) concentrations and lower cerebrospinal fluid (CSF) cortisol, indicating a lack of feedback inhibition for the release of the stress hormone cortisol (see Andersen & Teicher, 2009 for review). Similar results have been found in human studies which has been extensively reviewed by Sinha (2008), Shonkoff & Garner (2012), and Hölzel and colleagues (2011).
While the stress response system remains an important aspect in understanding addiction, psychological stress is also a common risk factor for relapse potential. Stress is typically a consequence from events or environmental conditions and manifested by acute psychological reactions where individuals seek a mollifying escape from the event, which is typically achieved through psychoactive substances. Mindfulness, however, has been posited to alleviate some of this psychological strain and aid in reductions in stress. For example, Creswell, Pacilito, Lindsay, and Brown (2014) found that exposure to a brief mindfulness intervention (compared to cognitive training) resulted in buffered self-reported psychological stress reactivity and increased cortisol reactivity in a lab-based stress test. In general, when under stress, our body activates an automatic or “auto pilot” response typically in the form of rumination, negative thoughts, assumptions about what will happen, and impulsivity (Esch, 2014). The MBRP curriculum has a strong focus on acknowledging when we enter ‘auto pilot’ and attempts to offer alternatives to remaining in this state. For example, one way MRBP may mitigate effects of stress is through the practice of reducing rumination and enhancing emotional regulation. Through practices such as the “SOBER breathing space” and allowing “thoughts to be thoughts” MBRP is teaching individuals not to push negative thought processes aside (which can activate a stress response via neglecting internal emotionality), but to sit with the negative thoughts in a safe space. Prior research has shown mindfulness to enhance positive emotional regulation strategies and self-compassion, to increase trait (or state) mindfulness, and decrease rumination and experiential avoidance (Chiesa et al., 2014).
The current study provides further support for the effects of mindfulness-based interventions on psychological stress, craving, and substance use among a sample of at-risk marginalized young adults. Further, MBRP may be an appropriate intervention for agencies to adopt, given proper training and supervision.
Acknowledgments: We are grateful to the National Institute on Drug Abuse (Grant number: 1R36DA041538; PI: Davis), the Fahs-Beck Fund for Research and Experimentation (PI: Davis, 082876), and the Campus Research Board (Grant number: RB15434; PI: Roberts) for funding the current study. We want to thank our research assistants Emily Hartung and Samantha Allen for their help with data collection and data entry.
References
Andersen, S. L., & Teicher, M. H. (2009). Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neuroscience and Biobehavioral Reviews, 33(4), 516–24.
Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–43.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., . . . & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–41.
Bonnie, R. J., Stroud, S., Breiner, H. (2015). Investing in the health and well-being of young adults. Washington, DC: National Academies Press.
Bowen, S., Chawla, N., Collins, S. E., Witkiewitz, K., Hsu, S., Grow, J., . . . Marlatt, G. A. (2009). Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse, 30(4), 295–305.
Bowen, S., Chawla, N., Marlatt, G. A. (2010). Mindfulness-based relapse prevention for addictive behaviors: A clinician’s guide. New York, NY: Guilford Press.
Bowen, S., Witkiewitz, K., Chawla, N., & Grow, J. (2011). Integrating mindfulness meditation and cognitive behavioral traditions for the long-term treatment of addictive behaviors. Journal of Clinical Outcomes Management, 18(10), 473–9.
Bowen, S., Witkiewitz, K., Clifasefi, S. L., Grow, J., Chawla, N., Hsu, S. H., . . . & Larimer, M. E. (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71(5), 547–56.
Brewer, J. A., Bowen, S., Smith, J. T., Marlatt, G. A., & Potenza, M. N. (2010). Mindfulness-based treatments for co-occurring depression and substance use disorders: What can we learn from the brain? Addiction, 105(10), 1698–706.
Brewer, J. A., Elwafi, H. M., & Davis, J. H. (2013). Craving to quit: Psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychology of Addictive Behaviors, 27(2), 366–79.
Brewer, J. A., Sinha, R., Chen, J. A., Michalsen, R. N., Babuscio, T. A., Nich, C., . . . Rounsaville, B. J. (2009). Mindfulness training and stress reactivity in substance abuse: Results from a randomized, controlled, stage I pilot study. Substance Abuse, 30(4), 306–17.
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–48.
Chiesa, A., Anselmi, R., & Serretti, A. (2014). Psychological mechanisms of mindfulness-based interventions: What do we know? Holistic Nursing Practice, 28(2), 124–48.
Cohen, S., Hamrick, N., Rodriguez, M. S., Feldman, P. J., Rabin, B. S., & Manuck, S. B. (2002). Reactivity and vulnerability to stress-associated risk for upper respiratory illness. Psychosomatic Medicine, 64(2), 302–10.
Cohen, S., Janicki-Deverts, D., & Miller, G. E. (2007). Psychological stress and disease. JAMA, 298(14), 1685–7.
Creswell, J. D., Pacilio, L. E., Lindsay, E. K., & Brown, K. W. (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12.
Davis, J. P., Smith, D. C., & Briley, D. A. (2017). Substance use prevention and treatment outcomes for emerging adults in noncollege settings: A meta-analysis. Psychology of Addictive Behaviors, 31(3), 242–54.
Edwards, E. R., Cohen, M. G., & Wupperman, P. (2016). Substance-treatment professionals’ perceived barriers to incorporating mindfulness into treatment. Substance Use & Misuse, 51(14), 1930–5.
Esch, T. (2014). The neurobiology of meditation and mindfulness. In S. Schmidt & H. Walach (Eds.), Meditation-neuroscientific approaches and philosophical implications (pp. 153–73). Cham, Switzerland: Springer International Publishing.
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60.
Gordon, H. W. (2002). Early environmental stress and biological vulnerability to drug abuse. Psychoneuroendocrinology, 27(1–2), 115–26.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–59.
Li, W., Howard, M. O., Garland, E. L., McGovern, P., & Lazar, M. (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96.
McEwen, B. S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338(3), 171–9.
McNiel, D. E., Binder, R. L., & Robinson, J. C. (2014). Incarceration associated with homelessness, mental disorder, and co-occurring substance abuse. Psychiatric Services, 56(7), 840–6.
Substance Abuse and Mental Health Services Administration (SAMHSA). (2013). Treatment episode data set (TEDS): 2001–2011. State admissions to substance abuse treatment services. Retrieved from https://www.samhsa.gov/data/sites/default/files/TEDS2011St_Web/TEDS2011St_Web/TEDS2011St_Web.pdf
Substance Abuse and Mental Health Services Administration (SAMHSA). (2014). Results from the 2013 national survey on drug use and health: Summary of national findings. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf
Shonkoff, J. P., & Garner, A. S. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–46.
Sinha, R. (2007). The role of stress in addiction relapse. Current Psychiatry Reports, 9(5), 388–95.
Sinha, R. (2008). Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences, 1141(1), 105–30.
Traube, D. E., James, S., Zhang, J., & Landsverk, J. (2012). A national study of risk and protective factors for substance use among youth in the child welfare system. Addictive Behaviors, 37(5), 641–50.
Walters, S. T., Ondersma, S. J., Ingersoll, K. S., Rodriguez, M., Lerch, J., Rossheim, M. E., & Taxman, F. S. (2014). MAPIT: Development of a web-based intervention targeting substance abuse treatment in the criminal justice system. Journal of Substance Abuse Treatment, 46(1), 60–5.
White, H. R., Labouvie, E. W., & Papadaratsakis, V. (2005). Changes in substance use during the transition to adulthood: A comparison of college students and their noncollege age peers. Journal of Drug Issues, 35(2), 281–306.
Witkiewitz, K., & Bowen, S. (2010). Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology, 78(3), 362–74.
Witkiewitz, K., Bowen, S., Douglas, H., & Hsu, S. H. (2013). Mindfulness-based relapse prevention for substance craving. Addictive Behaviors, 38(2), 1563–71.
Witkiewitz, K., Warner, K., Sully, B., Barricks, A., Stauffer, C., Thompson, B. L., & Luoma, J. B. (2014). Randomized trial comparing mindfulness-based relapse prevention with relapse prevention for women offenders at a residential addiction treatment center. Substance Use & Misuse, 49(5), 536–46.
Zgierska, A., Rabago, D., Zuelsdorff, M., Coe, C., Miller, M., & Fleming, M. (2008). Mindfulness meditation for alcohol relapse prevention: A feasibility pilot study. Journal of Addiction Medicine, 2(3), 165–73.
Editor’s Note: This article was adapted from an article by the same authors previously published in the Journal of Substance Abuse Treatment (JSAT). This article has been adapted as part of Counselor’s memorandum of agreement with JSAT. The following citation provides the original source of the article:
Davis, J. P., Berry, D., Dumas, T. M., Ritter, E., Smith, D. C., Menard, C., & Roberts, B. W. (2018). Substance use outcomes for mindfulness-based relapse prevention are partially mediated by reductions in stress: Results from a randomized trial. Journal of Substance Abuse Treatment, 91, 37–48.
Jordan P. Davis, PhD, is an assistant professor at the USC Suzanne Dworak-Peck School of Social Work in the department of Children, Youth, and Families and the associate director of the USC Center for Artificial Intelligence in Society. He has devoted much of his career to interdisciplinary research that addresses substance use, violence exposure (e.g., PTSD), and developmental needs of marginalized and vulnerable populations. Davis also focuses on the utility and development of longitudinal data analyses in the structural equation modeling framework. Davis’ primary research focuses on substance use disorder treatment among marginalized youth.
Jessenia De Leon, BS, graduated from California State University Long Beach with a BS in criminology, criminal justice, and emergency management. She is currently attending the University of Southern California and pursuing a dual-degree program (master’s/PhD) in social work. Her general interests include adolescent development, juvenile justice, and mindfulness interventions.











 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.