LOADING
Share

Motivational interviewing (MI) is a brief counselling intervention designed to increase motivation to change alcohol and drug use (Miller & Rollnick, 2012). Though it was originally designed as an intervention narrowly focused on problem drinking (Miller, 1985), MI has grown to become a broadly generalizable approach used to address a variety of problems. Research of MI for substance abuse has shown that it is effective, though there is less evidence of its long-term impact (Smedslund et al., 2011). However, few studies have extended MI beyond three or four sessions even though there is indication that higher doses of MI may result in improved outcomes (Burke, Arkowitz, & Menchola, 2003). This article describes the conceptualization and implementation of intensive motivational interviewing (IMI), a manual driven, nine-session delivery of MI for substance abuse (Polcin, Brown & Galloway, 2005). In addition, we present outcomes of a randomized study comparing IMI with a standard, single session of MI (SMI). Although the study was designed primarily to address the effectiveness of IMI for persons with methamphetamine (MA) dependence, we report important effects for drinking among women.
Much of the evidence for the efficacy of MI stems from the alcohol treatment literature with MI administered over one to four sessions (Heather, Rollnick, Bell, & Richmond, 1996; Project MATCH Research Group, 1997; Sellman, Sullivan, Dore, Adamson, & MacEwan, 2001). However, the impact of MI for persons with other drug use disorders is less clearly understood. MI for drug using populations is typically used as a preparation for more intensive treatment rather than a standalone intervention (Bien, Miller, & Boroughs, 1993; Brown & Miller, 1993). Interestingly, few studies have addressed the potential benefit of increasing the number of MI sessions to enhance motivation for change. Below we discuss the creation and implementation of IMI and research outcomes.
Conceptualization of IMI
IMI was conceptualized as a way to help clients with illicit drug disorders benefit from a larger dose of MI (Polcin, Galloway, Palmer, & Mains, 2004). The philosophy and techniques for IMI draw from the work of William Miller and colleagues (Miller & Rollnick, 2002). Like MI, IMI promotes the view that motivation will increase when the client and therapist form a collaborative relationship, openly exploring the benefits and consequences associated with substance use. Resistance to acknowledging substance use problems is met with reflection or examination of the role that substance use plays in the client’s life. This method of “rolling with resistance” contrasts with more confrontational approaches that attempt to “break down denial” or convince the client that he or she has a problem.
Of central importance is the spirit of collaboration with the client that leads to exploration of the role of substance use in their lives, the benefits and consequences, and what, if anything, the client might want to change. To a degree, IMI draws on the stages of change derived from the transtheoretical model (Prochaska, DiClemente, & Norcross, 1992). Therapists adapt interventions to the client’s stage of change, although there is acknowledgment that the stages of change are dynamic and fluid. Relapse is understood as a potential opportunity to help clients understand the role that substances play in their lives, and to examine what changes, if any, they wish to make. Therapists are instructed to use the fundamental techniques employed by MI:
- Reflective listening
- Summarizing
- Open questions
- Affirming self-efficacy
- Rolling with resistance
- Fostering collaboration
- Feedback/giving information
- Heightening discrepancies
- Eliciting self-motivating statements
- Change planning
While a full discussion of MI techniques is beyond the scope of this paper, readers wishing for more information should see Miller and Rollnick (2002).
IMI Manual Outline
The IMI manual (Polcin et al., 2005) was constructed so as to provide a general outline of the objectives and focus for each session as briefly outlined below. However, the manual was also designed to be sufficiently flexible to enable practitioners to address the issues they felt were of high importance throughout the counseling process. Thus, while the techniques and spirit of MI were consistently applied throughout the process, the content of sessions had some room for variation depending on issues that clients present. The goal was to make IMI clinically appealing and easily generalized. All of the aforementioned MI techniques were applied to all of the sessions based on the needs of the clinical situation. For a description of how to apply supportive and directive techniques prescriptively based on clinical considerations, see Polcin, Sterling, Brown, Brown, Buscemi, and Korcha (2014).
Session One
Before the first session begins, clients complete worksheets designed to facilitate discussion of presenting problems and stages of change. Questions ask about the types of problems clients are experiencing and their motivation to address them. The therapist generally begins by inviting clients to share their reasons for seeking treatment. The goal is to convey an overall tone that the session is a collaborative relationship that examines the role of substance use in the clients’ lives. A critical therapeutic task is to help clients feel comfortable, open, and honest about all aspects of their current situation, including substance use. Typically, techniques such as open-ended questions, affirmations, reflective listening, and summarizing are used liberally to help engage clients and form collaboration. The therapist has flexibility regarding when they choose to review the written worksheets, but they should be discussed before the session closes. Goals for this session are to build rapport, foster collaboration, facilitate client awareness of problems and concerns related to substance use or recovery, and clarify the clients’ stage of change. However, the therapist also adjusts to meet the clients at their stage of change. For example, if a client enters treatment and during the first session expresses a desire to make changes in his or her alcohol or drug use, the therapist begins discussion about change planning, which is typically the focus of session three.
Session Two
Before beginning session two, clients complete worksheets for the second session, which are designed to elicit the pros and cons of using substances as well as the pros and cons of making changes in substance use. The goals for this session are to validate reasons for resisting change, facilitate client awareness about the benefits and costs associated with substance use and recovery activities, and clarify experiences of ambivalence.
Session Three
Rather than completing structured exercises before this session, clients and therapist together collaborate in developing the client “change plan” in the session. Generally, this session consists of identifying desired changes, strategies for achieving them, and challenges clients may face in enacting the plan.
Session Four
The session begins with a discussion of what has been accomplished in previous sessions and what has transpired since the last session. The goals are to collaborate and evaluate the status of the change plan and to examine ambivalence as clients attempt to enact their change plan. The change plan is adapted, expanded, and modified as goals are achieved, new problems are identified or as the result of client changes to goal or means for achieving them.
Sessions Five through Seven
These sessions continue the work described in session four. The change plan is revisited on a weekly basis and revised as necessary. The sessions typically begin with a review of the past week and any other issues clients wish to discuss. The therapist looks for opportunities to apply the change plan to the topics being addressed and the plan is modified or changed as needed. An important task throughout this process is to facilitate examination of ambivalence (i.e., the pros and cons) about implementation of the change plan.
Session Eight
Although this session begins in a similar manner to sessions four through eight, the therapist is careful to ensure that the issue of termination is initiated before the session ends. It is important to remember that clients may have had many different experiences with ending therapy, and with saying “goodbye” in general. The therapist invites clients to talk about their feelings and experiences of therapy and the fact that it will end after the next session. In a collaborative manner, the therapist and clients assess the overall status of the change plan and options for additional treatment elsewhere.
Session Nine
Termination is initiated with a summary of the clients’ path through the stages of change with specific successes noted. The clients might be asked to summarize their growth and successes with therapist adding to this summary. The therapist can revisit the structured exercises completed at the beginning of treatment to help focus the last discussion. The therapist should continue with the discussion started the previous week about saying goodbye. Both the therapist and the clients share feelings about termination. The therapist makes sure that clients discuss what important things, skills, and/or strategies they can take with them based on their experiences in therapy and while in therapy. Before the session ends, the therapist and clients discuss options for current or future treatment if needed.
To ensure therapists were adhering to the IMI manual and not drifting into other therapeutic styles, we used a method described by Nuro et al. (2005) at the Yale University Psychotherapy Development Center. All sessions were audio recorded and rated by expert reviewers to ensure adherence to the manual as well as a minimum level of competence in its implementation. For more details about adherence measures, see Nuro et al. (2005) or our previous paper on adherence procedures when studyng IMI (Galloway, Polcin, Kielstein, Brown, & Mendelson, 2007).
Pilot Testing IMI
The pilot testing of IMI began in 2005 with recruitment of thirty methamphetamine (MA) dependent individuals, all of whom received the nine-session intervention as a stand-alone treatment. Results showed statistically significant and clinically meaningful reductions of self-reported MA use as well as decreases in MA-positive urine samples during treatment (Galloway et al., 2007).
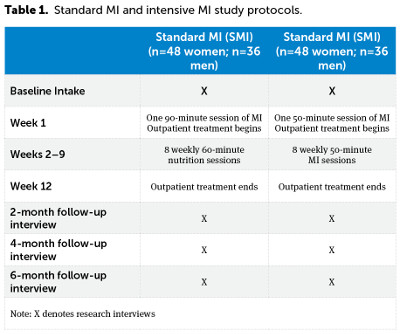
The promising pilot study outcomes led to the development of a study randomizing MA dependent individuals to either nine-sessions of IMI or to a single session of standard motivational interviewing (SMI). SMI clients also received eight sessions of nutritional education group so that both study conditions had time and attention equivalence. All study participants in both groups received twelve weeks of outpatient treatment consisting of three groups each week in addition to receipt of IMI or SMI. Study interviews were at treatment intake, and at two, four, and six months following intake. The study protocol is outlined in Table 1.
In addition to collecting demographic information, the assessment measures used for the present study included the DSM-IV Checklist for Drug and Alcohol Dependence (American Psychiatric Association, 2000; Forman, Svikis, Montoya, & Blaine, 2004) to determine dependence on MA, the Addiction Severity Index – Lite (ASI) (McLellan, Luborsky, Woody, & O’Brien, 1980) to assess the severity of drug and alcohol problems, and the Helping Alliance Questionnaire – II (HAQ) (Luborsky et al., 1996) to assess the strength of the therapeutic alliance.
The primary aim of the study was to examine whether IMI resulted in superior MA outcomes than SMI. Secondary aims included assessing the impact of IMI on other substances, including alcohol and other problems such as psychiatric symptoms. Results showed both treatment conditions substantially reduced their MA use during treatment and maintained decreased levels of MA use at six-month follow-up. However, there were no differences in MA use between clients assigned to IMI and SMI (Korcha, Polcin, & Bond, in press). Potential reasons for the similar MA outcomes for both study conditions as well as some areas where there were significant differences between the two conditions (e.g., psychiatric problems) are reviewed elsewhere (see Polcin et al., 2014).
Purpose of the Current Study
The purpose of this article is to report unexpected findings regarding alcohol outcomes. There were 164 individuals who reported problems with alcohol as well as MA. Alcohol problems were defined as having an ASI alcohol score above zero or reporting any alcohol dependence symptoms in the past twelve months at the baseline interview. We surmised that IMI might be more effective than SMI for other substances in addition to MA, including alcohol. However, we did not anticipate that alcohol outcomes would differ by gender. These findings, along with the study methods and implications for clinical practice are described below.
Sample Description
Demographically, approximately half of the study participants had never been married (50 percent). The mean age was thirty-eight (sd=10) years of age and over half (59 percent) had at least some college education. Most participants were white (68 percent) and over half (59 percent) met DSM-IV criteria for at least one other drug in addition to meeting criteria for MA dependence. Attendance to outpatient group meetings averaged fifteen sessions (sd=11) out of a total possible of thirty-six. No differences were evident between the IMI and SMI conditions or men and women within each of these conditions for any of the demographic variables or attendance to outpatient sessions. Attempts to locate and interview participants after they left treatment were successful. We contacted 95 percent at two months, 88 percent at four months, and 90 percent at six months.
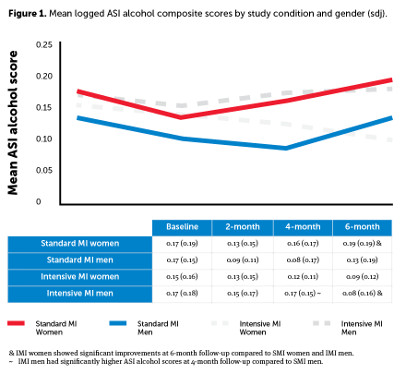
Outcomes at Four and Six Months
Figure 1 displays the mean logged alcohol ASI scores by treatment condition and gender. Longitudinal analyses were conducted using random effects modeling to estimate changes in alcohol ASI scores from baseline to each of the follow-up time periods. While no differences between condition and gender were apparent at the two-month interview, SMI men unexpectedly had lower ASI alcohol scores compared to the IMI men at the four-month interview. However, this effect did not continue at six months.
Differences in severity of alcohol problems between women receiving IMI and the other study groups emerged at four months and continued at six months. The only group that showed a lower ASI alcohol score at six months than at baseline was the women receiving IMI. Each of the other three groups had six-month scores that were equal to or higher than their baseline scores at the beginning of treatment. The six-month outcomes demonstrated that women receiving IMI had significantly lower ASI alcohol scores at this interview compared to women receiving SMI and men receiving IMI, although no differences were apparent when compared with the SMI men.
Therapeutic Alliance
Because IMI women showed significant improvement from baseline to six-month outcomes compared to IMI men and SMI women, we examined possibilities within session indicators of therapeutic alliance using the HAQ. The HAQ was administered immediately following each IMI and SMI treatment session. Figure 2 displays the mean scores of IMI men and women for every treatment session. IMI women showed significantly higher alliance mean scores at sessions six, seven, and eight compared to the men randomized to IMI.
Discussion on Results
Study results suggest there is potential benefit to providing more MI sessions than is typical when treating women with alcohol problems. While there were no differences between a single session of MI during treatment and nine sessions, women in the nine-session condition had better outcomes at the four-month follow-up. Moreover, the differences between the two groups became even larger at the six-month follow-up. For women receiving nine sessions of MI, improvements continued after treatment. In contrast, the women in standard MI resumed drinking to the point where their problems at six months were more serious than when they entered treatment. It is unclear why this delayed effect was found, but it is possible that IMI initiates a process of better management of various issues related to alcohol use that continues after treatment is completed. More research on women’s experiences during and after treatment would be helpful to understanding this delayed effect for IMI.
In the sections that follow we discuss key issues that may be relevant to the impact of IMI on alcohol outcomes for women. Each of the issues identified will require more research to understand thoroughly. However, we offer tentative considerations based on our current results, the existing literature, and reflection from our clinical work.
Co-Occurring Psychiatric Symptoms
One factor that might be relevant to the superior outcomes of IMI over SMI in the treatment of alcohol problems for women is the occurrence of psychiatric problems. Research has shown co-occurring psychiatric problems are common among women with receiving alcohol treatment, particularly problems with depression and anxiety (Cohen, Greenberg, Uri, Halpin, & Zweben, 2007; Greenfield et al., 2007; Tuchman, 2010). Moreover, well evidenced in the substance abuse literature is the relationship of physical or sexual trauma to subsequent substance abuse. Lifetime trauma rates are over 50 percent for women in alcohol or drug treatment programs (Haller & Miles, 2004; Lown, Nayak, Korcha, & Greenfield, 2011; Vogeltanz et al., 1999; Wilsnack, Vogeltanz, Klassen, & Harris, 1997). The women in the present study reported especially high rates of physical or sexual abuse histories (83 percent of SMI women, 93 percent of IMI women). It could be informative to hear women’s views about how IMI affected psychiatric symptoms during and after treatment. As described in the “Future Directions” section, we have plans to conduct this type of research.
Relative to standard MI, the more intensive nine-session model might allow for more work on co-occurring psychiatric symptoms that is more enduring. The IMI manual was designed to be flexible in terms of topics addressed and adaptive to the needs and preferences of clients. It therefore is able to readily address co-occurring problems such as psychiatric symptoms. The intent in designing the manual in this way was so that it could incorporate naturally occurring segues from topic to topic, including psychiatric problems (Hettema, Steele, & Miller, 2005).
Differential Effects for Alcohol and Methamphetamine
It is unclear why there appears to be a significant effect for IMI on alcohol problems among women, but no apparent effect on methamphetamine. This is another area in need of more research. However, different reasons for using these substances could be one factor. A variety of papers—such as Polcin et al., 2012—suggest that MA use among women is often rooted in body image problems that can result in disorders such as bulimia and somatoform. In addition, MA use among women often occurs within the context of intimate relationships, many of which involve coercion to use MA and physical or sexual abuse. Studies suggest the reasons women drink are different. For example, it has long been known that alcohol-dependent women frequently present serious problems with anxiety and depression that fuel drinking (Greenfield et al., 2007). It is plausible that IMI might be more helpful for these co-occurring disorders than for the body image disorders and abusive relationship dynamics associated with MA dependence. In addition, our analysis of audiotape therapy sessions suggested discussion of anxiety and depression were more common than discussion of somatoform issues or pressure to use from intimate partners.
Reflection on Gender Effects
The different effect of IMI by gender is another issue that needs to be better understood. However, our current preliminary findings add to a growing body of work supporting relational theory (De Young, 2003) as an explanation for how women benefit from psychotherapy. Many types of psychotherapy focus on separation, autonomy, and self-efficacy as therapeutic objectives. In contrast, relational theory emphasizes building interpersonal connection with the therapist and with others in the client’s social sphere. From this perspective, self-efficacy, self-esteem, and perhaps reduction in drinking, are built more from interpersonal connection with others than autonomy or use of skills to manage problems.
We posit that MI’s emphasis on an empathic, collaborative relationship as an essential component in the healing process is consistent with relational theory and that may be one reason we see a beneficial response to higher doses of MI among women. Our findings assessing the therapeutic alliance among women receiving IMI lend additional support to relational theory. We found women tended to have stronger therapeutic alliances than men and those alliances increased over time in the IMI condition. Further, the level of therapeutic alliance was associated with better alcohol outcome.
Limitations
There are a number of limitations that need to be noted:
- It needs to be emphasized that the women who made improvements on alcohol problems also had dependence on MA. It remains to be seen whether women with alcohol problems who did not have co-occurring MA dependence would make similar improvements.
- Data were collected at one treatment site in Northern California and there could be variation among different programs or different parts of the country. In addition, there were a total of three therapists employed for the study and results could differ with a larger number of therapists providing treatment.
- Data on alcohol was self-report and not confirmed by urine or blood analysis.
Future Directions
The next step of research on IMI is currently underway. Our team at the Alcohol Research Group has been funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to study IMI for alcohol-dependent women. Unlike the current study, we will be targeting women exclusively and they will need to by currently dependent on alcohol to be included. In this article we have speculated about potential reasons IMI was effective for women, but not men, and alcohol, but not MA. To sufficiently understand these questions we need to hear from the women themselves. Thus, in the new study we have plans to interview women after treatment and at twelve-month follow-up. We will ask questions about how IMI was helpful and not helpful during treatment, how the intervention affected their ability to limit or abstain from drinking during and after treatment, and how the intervention affected psychiatric symptoms such as anxiety and depression. Within these discussions we will be looking for ways the women’s experiences confirm and refute the relational theory (DeYoung, 2003) of how women change during psychotherapy. Finally, we will ask about issues largely ignored in the current alcohol treatment literature, such as client perceptions about specific MI interventions; the perceived effects of “critical sessions” that result in sudden changes; factors perceived to influence the therapeutic alliance and within session experiences; external factors outside of treatment that are perceived to influence drinking; and ways therapists adapt IMI in response to client needs and experiences during treatment.
References
American Psychiatric Association (Ed.). (2000). Diagnostic and statistical manual for mental disorders (4 ed.). Washington, DC: Author.
Bien, T. H., Miller, W. R., & Boroughs, J. M. (1993). Motivational interviewing with alcohol outpatients. Behavioural and Cognitive Psychotherapy, 21(4), 347–56.
Brown, J. M., & Miller, W. R. (1993). Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors, 7(4), 211–8.
Burke, B. L., Arkowitz, H., & Menchola, M. (2003). The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology, 71(5), 843–61.
Cohen, J. B., Greenberg, R., Uri, J., Halpin, M., & Zweben, J. E. (2007). Women with methamphetamine dependence: research on etiology and treatment. Journal of Psychoactive Drugs, Suppl. 4, 347–51.
DeYoung, P. A. (2003). Relational Psychotherapy. A primer. Toronto, Ontario, Canada: Brunner-Routledge.
Forman, R. F., Svikis, D., Montoya, I. D., & Blaine, J. (2004). Selection of a substance use disorder diagnostic instrument by the National Drug Abuse Treatment Clinical Trials Network. Journal of Substance Abuse Treatment, 27(1), 1–8.
Galloway, G. P., Polcin, D. L., Kielstein, A., Brown, M., & Mendelson, J. (2007). A nine-session manual of motivational enhancement therapy for methamphetamine dependence: adherence and efficacy. Journal of Psychoactive Drugs, Suppl. 4, 393–400.
Greenfield, S. F., Brooks, A. J., Gordon, S. M., Green, C. A., Kropp, F., McHugh, R. K., . . . Miele, G. M. (2007). Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence, 86(1), 1–21.
Haller, D. L., & Miles, D. R. (2004). Personality disturbances in drug-dependent women: relationship to childhood abuse. The American Journal of Drug and Alcohol Abuse, 30(2), 269–86.
Heather, N., Rollnick, S., Bell, A., & Richmond, R. (1996). Effects of brief counselling among male heavy drinkers identified on general hospital wards. Drug and Alcohol Review, 15(1), 29–38.
Hettema, J., Steele, J., & Miller, W. R. (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1, 91–111.
Korcha, R., Polcin, D. L., & Bond, J. (in press). Social influences as moderators of motivation to abstain from alcohol and drugs. Addictive Behaviors.
Lown, E. A., Nayak, M. B., Korcha, R. A., & Greenfield, T. K. (2011). Child physical and sexual abuse: a comprehensive look at alcohol consumption patterns, consequences, and dependence from the National Alcohol Survey. Alcoholism: Clinical and Experimental Research, 35(2), 317–25.
Luborsky, L., Barber, J. P., Siqueland, L., Johnson, S., Najavits, L. M., Frank, A., & Daley, D. C. (1996). The revised Helping Alliance Questionnaire (HAq-II). Journal of Psychotherapy Practice and Research, 5(3), 260–71.
McLellan, A. T., Luborsky, L., Woody, G. E., & O’Brien, C. P. (1980). An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. The Journal of Nervous and Mental Disease, 168(1), 26–33.
Miller, W. R. (1985). Motivation for treatment: A review with special emphasis on alcoholism. Psychological Bulletin, 98(1), 84–107.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people for change (2nd ed.). New York, NY: Guilford Press.
Miller, W. R., & Rollnick, S. (2012). Motivational interviewing: Helping people change (3rd ed.). New York, NY: Guilford Press.
Nuro, K. F., Maccarelli, L., Martino, S., Ball, S. A., Baker, S. M., Rounsaville, B. J., & Carroll, K. M. (2005). Yale Adherence and Competence Scale (YACSII) Guidelines (2nd ed.). Retrieved from http://mirecc.va.gov/MIRECC/visn1/docs/products/Yale_Adherence_and_Competence_Scale_II_Guidelines.pdf
Polcin, D. L., Brown, M., & Galloway, G. P. (2005). Intensive motivational enhancement therapy manual. Berkeley, CA: Alcohol Research Group.
Polcin, D. L., Buscemi, R., Nayak, M., Korcha, R., & Galloway, G. (2012). Sex differences in psychiatric symptoms among methamphetamine-dependent residents in sober living houses. Addictive Disorders and Their Treatment, 11(2), 53–63.
Polcin, D. L., Galloway, G. P., Palmer, J., & Mains, W. (2004). The case for high-dose motivational enhancement therapy. Substance Use and Misuse, 39(2), 331–43.
Polcin, D. L., Sterling, J., Brown, T., Brown, M., Buscemi, R., & Korcha, R. (2014). Client and therapist views about intensive and standard motivational interviewing. Journal of Contemporary Psychotherapy. doi:10.1007/s10879-014-9280-1.
Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change. Applications to addictive behaviors. American Psychologist, 47(9), 1102–14.
Project MATCH Research Group. (1997). Matching alcoholism treatment to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol, 58(1), 7–29.
Sellman, J. D., Sullivan, P. F., Dore, G. M., Adamson, S. J., & MacEwan, I. (2001). A randomized controlled trial of motivational enhancement therapy (MET) for mild to moderate alcohol dependence. Journal of Studies on Alcohol, 62(3), 389–96.
Smedslund, G., Berg, R. C., Hammerstrom, K. T., Steiro, A., Leiknes, K. A., Dahl, H. M., & Karlsen, K. (2011). Motivational interviewing for substance abuse. The Cochrane Database of Systematic Reviews, 5.
Tuchman, E. (2010). Women and addiction: The importance of gender issues in substance abuse research. Journal of Addictive Diseases, 29(2), 127–38.
Vogeltanz, N. D., Wilsnack, S. C., Harris, T. R., Wilsnack, R. W., Wonderlich, S. A., & Kristjanson, A. F. (1999). Prevalence and risk factors for childhood sexual abuse in women: national survey findings. Child Abuse and Neglect, 23(6), 579–92.
Wilsnack, S. C., Vogeltanz, N. D., Klassen, A. D., & Harris, T. R. (1997). Childhood sexual abuse and women’s substance abuse: National survey findings. Journal of Studies on Alcohol, 58(3), 264–71.
Editor’s Note: This article was adapted from an article by the same authors previously published in the Journal of Substance Abuse Treatment (JSAT). This article has been adapted as part of Counselor’s memorandum of agreement with JSAT. The following citation provides the original source of the article:
Korcha, R. A., Polcin, D. L., Evans, K., Bond, J. C., & Galloway, G. P. (2014). Intensive motivational interviewing for women with concurrent alcohol problems and methamphetamine dependence. Journal of Substance Abuse Treatment, 46(2), 113–9.







 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.