LOADING
Share

Cannabis use is the most commonly used illicit substance in the United States, with approximately 8.4 percent of the population aged twelve and older reporting current use (SAMHSA, 2014). Heavy cannabis use can lead to a variety of negative consequences. In particular, research has highlighted the links between long-term use and declines in cognitive functioning, physical and emotional health, and occupational status (Hall, 2014; Stephens & Banes, 2013). Thus, there is a need to develop and implement interventions for cannabis-using populations.
A variety of treatments exist for substance use, including Twelve Step interventions, family-based therapies, contingency management, motivationally based approaches, and skills-based interventions. Among cannabis-using populations, therapeutic interventions that have integrated motivational enhancement therapy (MET) and cognitive behavioral therapy (CBT) have been shown to be especially efficacious (Budney, Higgins, Radonovich, & Novy, 2000; Copeland, Swift, Roffman, & Stephens, 2001; Stephens, Roffman, & Curtin, 2000). MET is designed to elicit and bolster motivation for change by providing personalized feedback in tandem with an opportunity to think candidly with nonjudgemental counselors about how risky behavior is affecting clients’ lives. CBT is designed to assess and change maladaptive thoughts, feelings, and behaviors and teach skills to avoid substance use and instead utilize more helpful coping strategies. This combination of MET and CBT has been found to be successful for the treatment of cannabis disorders in a variety of studies. A large, multisite trial found that nine sessions of MET/CBT were more effective in reducing problematic use than a two-session MET-only intervention (MTPRG, 2004). This study on brief treatments for cannabis dependence resulted in a published treatment manual (Steinberg et al., 2005). Although efficacious treatments for cannabis dependence have been identified, abstinence rates tend to be in the range of 20 to 40 percent and decrease over time. Thus, research on augmenting the effects of these treatments and extending gains through longer-term follow-ups is needed.
Research has suggested that the standard of care for substance use intervention should include continued monitoring over time (McKay, 2005, 2006). Follow-up care that is personalized to the needs of the individual and flexible (Brown, Seraganian, Tremblay, & Annis, 2002; Stout, Rubin, Zwick, Zywiak, & Bellino, 1999) may prevent attrition from ongoing care (McKay et al., 2010). Evidence for the role of continued care in substance use comes from literature on recovery management checkups (RMC), which found that postdischarge relapsers from outpatient and inpatient treatment centers who were reengaged using motivational interviewing (MI) were more likely to reenter treatment and less likely to need substance use treatment at two-year follow-up (Dennis, Scott, & Funk, 2003; Scott, Dennis, & Foss, 2005).
The Study
With the goal of improving treatment outcomes for cannabis dependence, maintenance check-ups (MCUs) were designed to reinforce progress made in treatment, identify those participants who were struggling, and increase motivation for change and engagement in treatment sessions for those needing continued support. All participants received a standard, nine-session MET/CBT treatment. In addition, all participants were given the option of continuing MET/CBT treatment with their original therapist as needed. Half of the participants received MCUs at one and three months after the completion of the initial treatment period for the purpose of bolstering the success of the initial base treatment. Those in the no check-up condition (NCU) did not receive these check-ups. We reassessed participants after the base treatment (three-month follow-up) and six months later (nine-month follow-up). We hypothesized that:
- Participants in both conditions—that is, with and without extra check-up sessions—would reduce cannabis use and associated problems following the initial nine sessions of MET/CBT treatment, replicating previous findings.
- Those who received extra check-ups (MCU condition) would reduce their use and related consequences more than those without the check-up sessions (NCU condition).
- Some of the greater improvement in the MCU condition would be due to greater utilization of additional MET/CBT sessions following the check-up sessions.
Design and Participants
Participants were recruited via newspaper and radio advertisements from the Seattle, Washington metropolitan area. The study advertisement specifically offered treatment for cannabis use. The following elements of the study occurred prior to any treatment administration: eligibility screening, first via brief phone screening, then in-person baseline interview; informed consent; administration of structured interview and self-report questionnaires; and final eligibility determination.
In five months, 228 people called and expressed interest in this cannabis treatment trial. A total of seventy-four participants were eligible and were randomly assigned to either the MCU (n = 37) or NCU (n = 37) intervention condition. The participants were male (66 percent), Caucasian (78 percent), had a mean age of 37.73 (SD = 12.08) years old, and had an average of 14.19 (SD = 2.63) years of education. Most had never married (46 percent) or were divorced or separated (23 percent).
Participants were excluded from the study if they used cannabis on fewer than fifty of the last ninety days, did not meet diagnostic criteria for cannabis dependence, were already engaged in treatment, met diagnostic criteria for alcohol or other drug dependence, lived more than sixty miles from the study site, were currently exhibiting symptoms of psychosis, were under the age of eighteen or planned to relocate during the course of the study.
Assessment Procedures
The following measures were utilized in this study:
- Timeline Follow-Back (Sobell & Sobell, 1992): assessed cannabis use frequency. Percentage of days of use in the past thirty days was calculated. Self-reported cannabis use was verified via urine screen.
- Marijuana Problems Scale (MPS; Stephens et al., 2000): assessed nineteen negative consequences commonly associated with cannabis use.
- The Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1996): assessed substance use dependence and was used to screen for psychotic symptoms.
- Situational Self-Efficacy Scale (Stephens, Wertz, & Roffman, 1995): assessed confidence in avoiding cannabis via a twenty-item scale.
Participants were compensated $50 for completing each of the follow-up research interviews at three and nine months and an additional $50 if they completed both follow-up assessments.
Therapy Procedures
All participants received nine sessions of MET/CBT over the first three months of the trial, as outlined in previous research (MTPRG, 2004; Steinberg et al., 2005). All participants were offered the option of additional MET/CBT treatment sessions through the six months following the completion of the base treatment as needed. Participants in the MCU condition also received two check-up sessions at one and four months following the completion of the base treatment (i.e., at the four- and seven-month anniversaries of the baseline assessment). Participants were reassessed immediately after base treatment (three months after baseline study enrollment) and six months after base treatment (nine months after baseline).
Base Treatment
The base treatment was comprised of nine sessions (MTPRG, 2004; Steinberg et al., 2005). The first two sessions were focused on MET, which included MI plus the provision of personalized feedback related to cannabis use. A personalized feedback report was created for each of the participants, summarizing information they reported in the baseline assessment. Feedback domains included frequency and patterns of cannabis use, money spent on cannabis, how their use compared with others their age in the United States, cannabis abuse and dependence symptoms, and life goals. Counselors reviewed this personalized feedback report with participants in their first two sessions, utilizing MI techniques throughout. Subsequent sessions utilized both MET and CBT components to address participants’ individual needs. Core CBT modules included understanding use, coping with cravings, managing thoughts about use, problem solving, and refusal skills. Details about this treatment can be found in the published manual (Steinberg et al., 2005).
Optional Sessions
All participants had access to optional MET/CBT treatment sessions as needed throughout the course of the project. For these sessions, modules from the same manual were selected based on participants’ current concerns. The purpose of these sessions was to provide reinforcement for participants who felt they needed additional assistance in achieving or maintaining their cannabis use goals.
Maintenance Check-Up Sessions
In addition to the base treatment and optional additional sessions, MCU condition participants had two maintenance check-up sessions at one and three months after completing the base treatment. These sessions included a brief computerized assessment and personalized feedback on any changes in overall rates of use, problems, and dependence symptoms since the previous base treatment sessions. Counselors delivered sessions in a MI-consistent style. Each PFR for each check-up included data from previous time points to allow the participant to visually see the progress they had made over time. The feedback was presented visually in order to illustrate change that had taken place and create opportunities for discussion. For example, reported days of use at baseline and check-ups one and two appeared in a line graph and served as a launching point to discuss changes in use (see Figure 1).
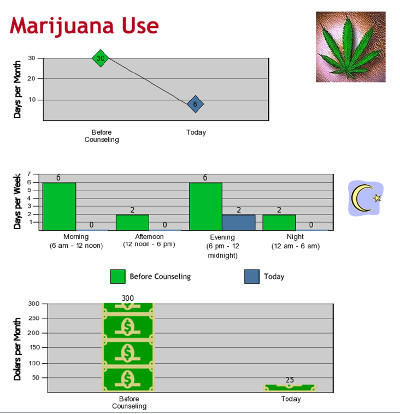
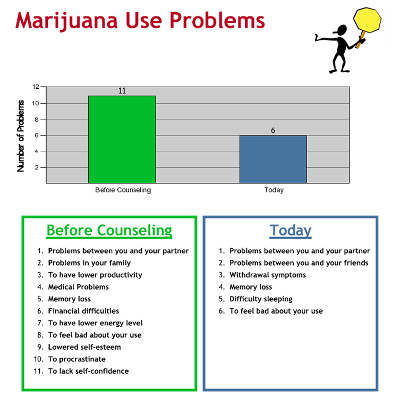

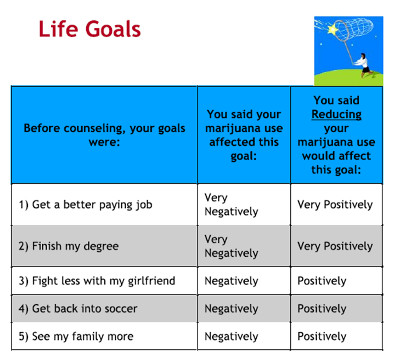
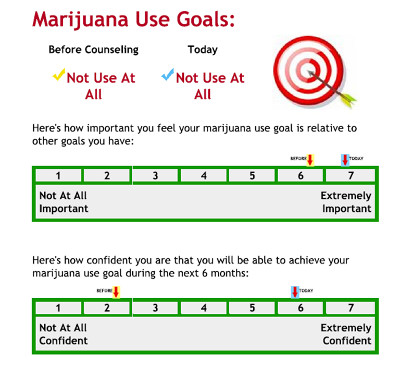
Additionally, counselors and participants discussed life goals and how their cannabis use or reduction in use affected the progress towards or away from each goal. Confidence and the importance of making changes in cannabis use were elicited from participants and discussed. The objective of these sessions depended on participants’ level of use. For participants whose use had stopped or significantly decreased the session’s target was to reinforce changes made in use and highlight the impact of these changes on their lives. If participants had stopped using completely, counselors offered affirmation of this accomplishment and asked for details on how they had made the change, how they were feeling about the change, and what benefits they’ve noticed, thereby providing the opportunity for participants to reflect on their accomplishment and strengthening motivation to continue. If they were still using regularly and experiencing problems, the PFR helped to elicit their feelings, disappointment, and concern, and by reflecting these concerns, helped to build motivation for further change.
Depending on the individual, some sessions focused on overall functional improvement or, in other cases, how cannabis was getting in the way of life goals and reasons for committing to making a change. For individuals who were experiencing high rates of problems or who were dissatisfied with the impact of their use on functioning, participants were reminded of and encouraged to attend the optional MET/CBT sessions.
Counselor Training and Supervision
Therapy was delivered by master’s level therapists who were trained for forty or more hours under the supervision of an experienced MET/CBT counselor. In addition to initial training, therapists also participated in ongoing weekly supervision throughout the course of the treatment study, in which recorded therapy sessions were reviewed for adherence to protocol. Therapists saw participants in both conditions.
Results
First, we wanted to ensure that subsequent analyses were not influenced by inequalities between conditions. Our analyses revealed no significant differences between the MCU and NCU conditions, meaning randomization created two equivalent groups. Secondly, we evaluated self-reported rates of cannabis use as compared to urinalysis results in order to determine the accuracy of self-report. Results indicated a high rate of agreement between the two measures, 87 percent at three months and 95 percent at nine months, which suggests that participants were responding truthfully. In sum, these preliminary analyses increase the confidence we have in the reported data and subsequent conclusions.
Analyses of Treatment Attendance
On average, participants completed the majority of the base treatment sessions (6.92 out of nine, SD = 3.15). Participants in both conditions attended a statistically similar number of sessions of base treatment. In the MCU condition, the majority of participants attended both check-up sessions—78 percent attended the first check-up, 81 percent attended the second check-up. Over half of participants in the MCU condition attended at least one of the additional, optional MET/CBT sessions (62 percent). Slightly fewer attended additional treatment sessions from the NCU condition (46 percent). The differences between these rates of attendance between conditions were not statistically significant, nor was the average number of optional CBT sessions attended (4.30 for MCU versus 2.81 for NCU). Overall, these findings do not strongly support our expectation that participation in the check-ups would lead to greater utilization of additional treatment.
Analyses of Treatment Outcome
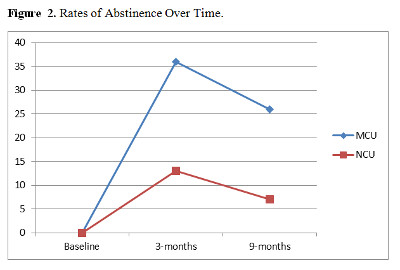
Our first hypothesis was that participants in both conditions would increase abstinence, reduce rates of use, and decrease the number of cannabis-related problems, so we included all participants in these analyses to determine the impact of base treatment. Results indicated that approximately 24.5 percent of participants at three months and 16.5 percent of participants at nine months reported abstinence over the previous month. Subsequent analyses evaluated the impact of treatment on days of cannabis use; results showed that participants in both conditions significantly reduced their cannabis use throughout the course of treatment and through the follow-up (F = 46.56; p < .001). These analyses were repeated to evaluate the impact of treatment on rates of dependence symptom and cannabis problem counts. Results showed that both conditions reduced their rates of cannabis dependence and problems over time (F = 41.20, p < .001 and F = 34.84, p < .001).
The next hypothesis stated that the two check-ups would augment, or better maintain, treatment gains, so we evaluated changes by condition. Individuals in the MCU condition were more likely to be abstinent than those in the NCU condition at the three-month time point (36 percent versus 13 percent; Χ2 (66) = 4.44; p < .05) and at the nine-month time point (26 percent versus 7 percent; Χ2 (63) = 3.72; p < .06) follow-ups (see Figure 2). However, there were no statistically significant differences in percentage of days of use over time as a function of condition (F = 2.76, p < .08). Further evaluation at each time point revealed that the MCU condition reported fewer days of cannabis use than the NCU condition at the three-month time point (posttreatment) relative to baseline (p < .05; d = 0.88). Although both conditions reduced problems and symptoms, results from analyses of cannabis-related problems and dependence symptoms indicated that rates did not significantly differ by condition.
The difference in rates of cannabis use between conditions at the three-month time point was not hypothesized. At this follow-up, the MCU condition had not received their additional check-ups. Thus, both conditions had received the same treatment. Additionally, the therapists were supervised on session content, meaning that there was little possibility of the treatment administration being fundamentally different between conditions. Exploratory analyses tested to see if self-efficacy, or participants’ confidence in their ability to abstain from cannabis use, could explain these differences between conditions before the check-ups occurred. Results indicated that individuals in the MCU condition endorsed a significantly higher rate of self-efficacy to abstain from use at the three-month follow-up than participants in the NCU condition (p < .05), even though the two groups did not differ in their reduction of marijuana use prior to that point.
The two groups of participants did not differ significantly in their use of MET/CBT sessions, so we did not test the hypothesis that treatment condition differences would be partially due to greater treatment attendance.
Discussion
This study evaluated the effectiveness of motivationally based check-up sessions in boosting treatment outcomes for individuals in treatment for cannabis dependence. Results revealed that all participants, regardless of whether or not they received the maintenance check-ups, experienced a significant decline in their rates of use, dependence symptoms, and problems associated with use. These findings are similar to other treatment trials that have utilized MET/CBT without the booster sessions (MTPRG, 2004), thus providing additional support for the utility of this combination among heavy-using, problematic cannabis consumers. Although many participants reengaged with their counselors after formal treatment had ended, taking advantage of the optional MET/CBT sessions, the MCUs did not stimulate a greater use of these sessions as originally predicted. This in combination with the very high attendance rates at the maintenance check-up sessions suggests that having further counseling support past the base treatment was attractive to many, regardless of condition.
A puzzling finding was that rates of cannabis abstinence in the MCU condition were higher and use was lower before the check-up sessions had taken place. We found that individuals in the MCU group had higher rates of self-efficacy, despite receiving the same treatment as the NCU condition until that point. Given that therapists were specifically evaluated on treatment protocol adherence during the base session treatment, this difference in self-efficacy could not be explained by session content. However, therapists were responsible for discussing check-ups for individuals in the MCU condition. They introduced the rationale behind the check-up sessions and prepared participants for the process of engaging in check-up sessions. Thus, one potential explanation for the difference in rates of cannabis use and abstinence among MCU participants prior to the check-up could be that the knowledge of obtaining future efficacious treatment could have increased self-efficacy or their belief in their ability to change their cannabis use. Given that self-efficacy has been found to be a robust predictor of treatment outcomes in cannabis treatment (Litt, Kadden, & Stephens, 2005; Stephens et al., 1995), this increase in self-efficacy among MCU participants could explain the increased rates of abstinence prior to the actual check-up session. It is also possible that participants who knew they would be checking in with their counselors one month after treatment anticipated some accountability for their progress. However, no measure was included to assess this.
Limitations
Some limitations of the current study should be noted. The number of participants in the study could have limited our statistical power to find differences in treatment outcomes. Differences could have been more pronounced at later follow-ups and with the addition of more check-up sessions. Future studies should utilize larger samples, additional check-up sessions, and longer follow-up periods to assess these potential limitations.
Conclusion and Summary
This study provides support for the use of MET/CBT interventions in the treatment of cannabis use disorder. Participants in both conditions decreased rates of use and problematic outcomes over time. Despite finding limited support for the benefits of adding check-up booster sessions, the study demonstrated that there is a clear need for treatments for cannabis use disorders and that the availability of aftercare or additional sessions is attractive and utilized by most. Overall, this study supports conceptualizing cannabis disorders as a chronic condition, and requires further work in identifying effective ways of providing treatment over time and reengaging those who may relapse following initial treatment.
References
Brown, T. G., Seraganian, P., Tremblay, J., & Annis, H. (2002). Matching substance abuse aftercare treatments to client characteristics. Addictive Behaviors, 27(4), 585–604.
Budney, A. J., Higgins, S. T., Radonovich, K. J., & Novy, P. L. (2000). Adding voucher-based incentives to coping skills and motivational enhancement improves outcomes during treatment for marijuana dependence. Journal of Consulting and Clinical Psychology, 68(6), 1051–61.
Copeland, J., Swift, W., Roffman, R., & Stephens, R. (2001). A randomized controlled trial of brief cognitive-behavioral interventions for cannabis use disorder. Journal of Substance Abuse Treatment, 21(2), 55–64.
Dennis, M., Scott, C. K., & Funk, R. (2003). An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning, 26(3), 339–52.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1996). Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV). Washington, DC: American Psychiatric Press.
Hall, W. (2014). What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction, 110(1), 19–35.
Litt, M. D., Kadden, R. M., & Stephens, R. S. (2005). Coping and self-efficacy in marijuana treatment: Results from the marijuana treatment project. Journal of Consulting and Clinical Psychology, 73(6), 1015–25.
Marijuana Treatment Project Research Group (MTPRG). (2004). Brief treatments for cannabis dependence: Findings from a randomized multisite trial. Journal of Consulting and Clinical Psychology, 72(3), 455–66.
McKay, J. R. (2005). Is there a case for extended interventions for alcohol and drug use disorders? Addiction, 100(11), 1594–610.
McKay, J. R. (2006). Continuing care in the treatment of addictive disorders. Current Psychiatry Reports, 8(5), 355–62.
McKay, J. R., Van Horn, D. H., Oslin, D. W., Lynch, K. G., Ivey, M., Ward, K., … Covilello, D. M. (2010). A randomized trial of extended telephone-based continuing care for alcohol dependence: Within-treatment substance use outcomes. Journal of Consulting and Clinical Psychology, 78(6), 912–23.
Scott, C. K., Dennis, M. L., & Foss, M. A. (2005). Utilizing recovery management checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug and Alcohol Dependence, 78(3), 325–38.
Sobell, L. C., & Sobell, M. B. (1992). Timeline followback: A technique for assessing self-reported alcohol consumption. In J. P. Allen & R. Z. Litten (Eds.), Measuring alcohol consumption: Psychosocial and biological methods (pp. 41–72). Totowa, NJ: Humana Press.
Steinberg, K. L., Roffman, R. A., Carroll, K. M., McRee, B., Babor, T. F., Miller, M., . . . Stephens, R. (2005). Brief counseling for marijuana dependence: A manual for treating adults. Rockville, MD: SAMHSA.
Stephens, R. S., & Banes, K. E. (2013). Cannabis and hallucinogens. In B. S. McCrady & E. E. Epstein (Eds.), Addictions: A comprehensive guidebook (2nd ed., pp. 121–40). New York, NY: Oxford University Press.
Stephens, R. S., Roffman, R. A., & Curtin, L. (2000). Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology, 68(5), 898–908.
Stephens, R. S., Wertz, J. S., & Roffman, R. A. (1995). Self-efficacy and marijuana cessation: A construct validity analysis. Journal of Consulting and Clinical Psychology, 63(6), 1022–31.
Stout, R., Rubin, A., Zwick, W., Zywiak, W., & Bellino, L. (1999). Optimizing the cost-effectiveness of alcohol treatment: A rationale for extended case monitoring. Addictive Behaviors, 24(1), 17–35.
Substance Abuse and Mental Heath Services Administration (SAMHSA). (2014). Results from the 2013 national survey on drug use and health: Summary of national findings. Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf








 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.