Share

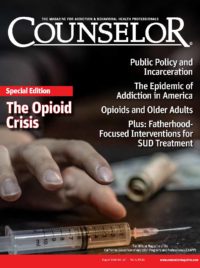
The medical community has been working to end the opioid crisis for years, but with 130 opioid overdose deaths every day (NIDA, 2019), it is clear that members of the treatment world and government need to break some bad habits.
We have serious problems with the way we treat opioid addiction, medically known as opioid use disorder (OUD), which stems from the widespread stigma surrounding treatments that break from the traditional, abstinence-only mold. The medical field—and policymakers—must recognize the effectiveness of evidence-based treatments over abstinence-only treatments and put an end to the biases surrounding many facets of addiction recovery. This will not only allow for more effective care, but it will provide clarity and motivation to revise antiquated policies.
First, effective treatment begins with proper recognition and classification of addiction. This means realizing it is a mental illness, not a moral failing. This is no small task because mental health has often been given lower priority than physical health at the policy and practical levels. As a result, the mental illnesses that underpin much of the opioid crisis are often left unconsidered or omitted by the current outdated treatment systems. Identifying and proactively treating the mental health aspect of addiction will be a tremendous help in fighting the opioid epidemic.
Second, we must get away from the one-size-fits-all addiction treatment model. All addictions are different, but OUD is entirely unique. Opioids alter a person’s brain chemistry in ways other substances do not, and ignoring the difference can be fatal for patients with OUD. Abstinence-only, talk-therapy treatments can work for those who have addictions to alcohol or some narcotics, but these programs yield an 80 percent relapse rate for those struggling with OUD. As individuals enter opioid withdrawal, their brain receptors change (Bart, 2012). When they relapse (as most do) and attempt to take their normal dose of opioids, their brains are overloaded, their bodies shut down and they perish.
There is a better way to treat people living with OUD and deal with this crisis, but we, as a nation, have to change the way we approach addiction and put scientific evidence over decades of stigma and bias.
Evidence-Based Treatment and Medication-Assisted Therapy
Evidence-based treatments implement traditional behavioral therapy and social support with what are known as “recovery medications” such as methadone, naltrexone and buprenorphine. This is known as “medication-assisted therapy” or “medication-assisted treatment” (MAT). This type of OUD treatment has produced astounding results. Compared to people not receiving MAT, opioid overdose deaths decreased by 59 percent for those receiving methadone and 38 percent for those receiving buprenorphine over the 12-month follow-up period research like this is the reasons MAT is endorsed by organizations such as the Centers for Disease Control and Prevention (CDC), the Office of National Drug Control Policy (ONDCP), the United Nations (UN) and the World Health Organization (WHO; NIH, 2018).
These treatments are clearly the most effective for attacking OUD, however less than 40 percent of eligible patients receive MAT (Volkow, Frieden, Hyde, & Cha, 2014). Less than half of treatment facilities even offer MAT and if they do, less than 35 percent of the patients are receive it (Volkow et al., 2014). The disparity is largely due to stigma associated with MAT. Some consider use of recovery medication as a form of “cheating” or exchanging one dependency for another. This attitude is incredibly harmful, and often fatal, to people living with addiction who have the courage to seek treatment.
This stigma against recovery medication must change. Based on the overwhelming number of Americans who are dying each day from opioid overdoses, we know that this addiction cannot be defeated by sheer willpower alone.
Laws and Health Care
Additionally, we must reverse absurd laws and misguided barriers that are founded on stigma and bias. Consider the following: any health care provider can prescribe opioids for pain but should that same health care provider seek to prescribe methadone or buprenorphine for addiction recovery, they must overcome a slew of regulatory barriers.
For instance, methadone—the first opioid recovery medication approved back in 1972— is held to an extremely high standard of distribution, which makes it tremendously challenging to help someone who is battling addiction and works for a living (IOM, 1995; DEA, 2019; SAMHSA, 2009). Distribution of methadone may only take place at federally regulated opioid treatment program (OTP) facilities, and most patients are required to travel daily to these facilities to be treated with their daily dose. The regulations OTPs jump through have ensured that the facilities offer additional services such as counseling, but these daily trips to facilities require time, transportation and an exceptionally flexible family and work life. Meanwhile, patients who need opioids for chronic illness or severe pain can simply get retail prescriptions to take home. Clearly, this is a double standard that is not rational given America’s current opioid crisis.
Buprenorphine, another recovery medicine, has its own barriers. The Drug Addiction Treatment Act of 2000 (DATA 2000) requires health care providers to complete an hours-long course and reach other qualifications to prescribe it (SAMHSA, 2019). The purpose of such a regulation was to prevent diversion (i.e., illegal and unintended use of the prescribed opioid medication). However, opioids for pain management, which can also be easily diverted (and have been a major contributor to the present epidemic), receive no such restriction and are held to a lower standard of prescription. Although recent legislation and action by the Trump administration has eased some of these restrictions, the additional hurdle of certification remains. When opioid overdose is killing more people than car crashes, would we continue with these barriers? Again, we have a double standard. At the very least, why would the government not insist that all prescribers of any opioid-related therapy receive the additional certification?
Perhaps the most far-reaching bureaucratic policy that is preventing recovery treatment to patients is the lack of insurance parity and the lack of parity enforcement. A Milliman report commissioned by the Mental Health Treatment and Research Institute found that, in forty-six states, insurance companies have been paying physical health care providers 20 percent better than addiction and mental health care providers for the same services (Melek, Perlman, Davenport, 2017; NCBH, 2017). Therefore, those battling addiction have fewer and more expensive options for treatment.
Conclusion
If we are going to overcome and put an end to the opioid epidemic that is devastating the lives, families and communities of Americans every day, we must combat bias and stigma, execute the policies and treatments that work and tear down decades of barriers and bad policy.
This is not a problem that Washington alone can solve. Every doctor, nurse, patient, family member and loved one affected by the opioid crisis must work to change the way we think and talk about OUD. It is a matter of life and death for millions of Americans, and we cannot afford to continue to perpetuate the cycle of bias.
References
- Bart, G. (2012). Maintenance medication for opiate addiction: The foundation of recovery. Journal of Addictive Diseases, 31(3), 207–25.
- Drug Enforcement Administration (DEA). (2019). Buprenorphine. (2019). Retrieved from https://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf
- Institute of Medicine (IOM). (1995). Federal regulation of methadone treatment. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK232108/
- Melek, S. P., Perlman, D., & Davenport, S. (2017). Addiction and mental health vs. physical health: Analyzing disparities in network use and provider reimbursement rates. Retrieved https://www.milliman.com/uploadedFiles/insight/2017/NQTLDisparityAnalysis.pdf
- National Council for Behavioral Health (NCBH). (2017). National Council for Behavioral Health statement on parity report issued by Milliman, Inc. Retrieved from https://www.thenationalcouncil.org/press-releases/national-council-behavioral-health-statement-parity-report-issued-milliman-inc/
- National Institute on Drug Abuse (NIDA). (2019). Opioid overdose crisis. Retrieved from https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis
- National Institutes of Health (NIH). (2018). Methadone and buprenorphine reduce risk of death after opioid overdose. Retrieved from https://www.nih.gov/news-events/news-releases/methadone-buprenorphine-reduce-risk-death-after-opioid-overdose
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2009). Incorporating alcohol pharmacotherapie into medical practice: Treatment improvement protocol TIP 49. Retrieved from https://store.samhsa.gov/system/files/sma13-4380.pdf
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2019). Buprenorphine waiver management. Retrieved from https://www.samhsa.gov/medication-assisted-treatment/training-materials-resources/buprenorphine-waiver
- Volkow, N. D., Frieden, T. R., Hyde, P. S., & Cha, S. S. (2014). Medication-assisted therapies—Tackling the opioid-overdose epidemic. New England Journal of Medicine, 370(22), 2063–6.

Newt Gingrich
Newt Gingrich is former Speaker of the House and author of Trump’s America: The Truth About Our Nation’s Great Comeback. He is the host of the “Newt’s World” podcast and an advisor to Advocates for Opioid Recovery.








 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.