LOADING
Share

Knowing about addiction is no longer enough to treat addiction. The more we know about addiction, the more we know that no addict or alcoholic has just one problem. Addiction treatment has changed from a very segregated model to a very integrative one. The demand to meet the challenges of treating today’s addict requires extensive cross-training of alcohol and addiction counselors. Additionally, it requires the cross-training of mental health and behavioral health counselors as well.
The Period of Segregation
Prior to the twentieth century America’s addiction to drugs other than alcohol was not considered a problem. Yes, there was the “soldier’s disease” due to injuries from the Civil War and the use of morphine to treat pain and the occurrence of dependency. During this time white middle class women also developed dependency on opiate products. The concept of addiction was not yet developed, but those dependent on alcohol were often treated differently due to the fact that alcoholism was originally poorly defined. The abuse of alcohol was defined as a crime in some circles while in others it was a moral problem. The alcoholic was often chastised and segregated from society. Alcoholics were often treated by incarceration or confined to mental wards, but not for alcoholism per se. Alcoholism was not seen as a mental problem, but rather that the alcoholic manifested some mental problem. Thus in many ways the foundation for segregation for alcohol and drug use in America began.
By the time the twentieth century began, alcohol use and drug use were considered two different issues. In fact, we still distinguish between alcohol and drug use. We still use the term “alcohol and other drugs” or “AOD.” During the mid-1950s and into the early 1960s, alcoholism was determined to be a disease. At that time no other drug dependence was considered to be a disease. Eventually, addiction in and of itself was accepted as a disease. However, there was definitely a separation of opinions about being addicted to alcohol as opposed to other drugs. Even within treatment programs themselves there was often de facto separation between alcohol abusers and drug abusers. During the mid-1970s I was the director of an alcohol and drug abuse program for the US Army at Fort Carson, Colorado. When I inherited the program there were separate treatment facilities and programs for alcoholic clients and other drug clients. I started World War III when I combined the programs! The world was just not ready to accept that addiction was addiction.
This same problem existed between the world of addiction as a disease and the world of mental illness. For the longest time each disease was considered to have multiple symptoms or problems, but they were considered to be a part of the disease itself. They were not seen as indicative of an accompanying disease or co-occurring disorders. The field of addiction and mental illness were originally miles apart. In the mid-1980s I experienced World War IV when I was asked to do a workshop in Michigan for mental health counselors and addiction counselors on dual disorders. The atmosphere in the workshop was very tense and I couldn’t identify the problem. Finally, during lunch I discovered that the mental health counselors were ordered to attend the training with the addiction counselors. They saw no need to attend and no relationship between the two. Not to defend the addiction counselors, but they did not feel the same way. However, I believe that it was the introduction of dual disorders to the addiction field that began to not only break the ice between the two professional fields, but also to appreciate the need for cross-training of both groups. One of the strongest indicators of the success of dual disorder cross training occurred during the 1990s when the classification of dual disorders was changed to co-occurring disorders. This happened when both sides realized that they were usually not dealing with only two issues, but rather with multiple diseases often simultaneously occurring. Obviously, the need for serious integration of diseases and cross-training had arrived. According to Baker, we have seen the development of three treatment systems to describe the developing relationship between addiction and mental illness (1991). The first is the Sequential Model which is treatment in only one system, then the other. The second is the Parallel Model, when treatment is in two systems simultaneously. The third is the Integrated Model in which treatment is in a single, unified, and comprehensive treatment program for co-occurring disorders.
Today’s Cross-Training Integrative Needs
What are the cross-training needs today in the addiction field? Obviously I could write about the cross-training needs in the mental health field as well, but I will address the addiction ones only. It should be kept in mind that cross-training is not for clinicians only, but also for administrators. This is especially true when the chief administrator began as a clinician. In today’s world, CEOs of addiction treatment facilities need to be business, marketing, evaluation, and finance leaders in addition to the knowledge and skills necessary for effective clinical treatment and patient recovery.
The following is a diagram of the various types and needs of cross-training.
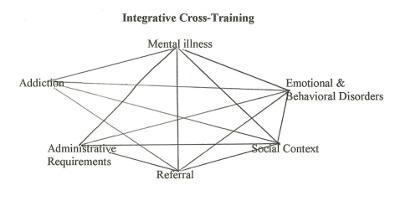
Each of the above areas focus on critical knowledge and skills that need to be developed in order to provide comprehensive, up-to-date treatment for addiction clients.
Addiction and Mental Illness Needs
The most important outcome of cross-training for addiction and mental illness professionals is to make correct diagnoses. We can no longer assume that all symptoms of addiction are attributable to the addiction or that all mental illness symptoms are attributable to only the mental illness. This is especially true when we remember that most addicts manifest between three to five mental illness symptoms. Also, the most common mental illnesses associated with addiction are depression, anxiety disorders, and bipolar disorders.
Emotional and Behavioral Disorders
The concept of addiction is being applied to more and more behavioral addictions. Some of these are referred to as process addictions such as gambling, compulsive spending, eating disorders, Internet addiction, and sex addiction. Additionally, emotional disorders such as adjustment disorders, attention deficit hyperactivity disorders, relationship problems, and posttraumatic stress disorders are associated with drug addiction.
Administrative Requirements
The amount of paperwork and reports required of clinicians and administrative personnel of treatment programs has increased dramatically in the past fifteen years due to new regulations of health care, legal requirements, funding requirements, and other types of documentation.
Social Context
The area of social context includes training in such things as gender considerations for differences in addiction, cultural and diversity considerations, environmental factors, occupational therapy, family considerations, and the impact of social policy. Social history of clients is not only becoming more and more important in developing therapeutic relationships with clients, but also in effectively treating the diverse populations of America.
Referral
Although cross-training within an addiction treatment program is vitally important, it is equally important to know when you need to refer clients to other supportive networks. This requires a good working knowledge of not only the other programs in your area, but also the necessary requirements for assistance and services.
Finally, one can ask if the addiction treatment field is getting more complicated or if we have developed a greater understanding of the complexity of addiction and the necessary support for treatment and recovery. Obviously, we are learning more and this has increased the necessity for integrative cross-training on a regular basis for all personnel serving addicted clients and their families.
References
Baker, F. (1991). Coordination of alcohol, drug abuse, and mental health services. Technical Assistance Publication Series Number 4. Washington, DC: Office for Treatment Improvement, Alcohol, Drug Abuse, and Mental Health Administration.
Previous Article
On Being a Mentor
Next Article
Special Feature – Grief and LossBy Holly Mack









 Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.
Counselor Magazine is the official publication of the California Association of Addiction Programs and Professionals (CCAPP). Counselor offers online continuing education, article archives, subscription deals, and article submission guidelines. It has been serving the addiction field for more than thirty years.